11.5 Bone Growth, Remodeling, and Repair
Created by CK-12 Foundation/Adapted by Christine Miller

Break A Leg
Did you ever break a leg or other bone, like the man looking longingly at the water in this swimming pool (Figure 11.5.1)? Having a broken bone can really restrict your activity. Bones are very hard, but they will break (or fracture) if enough force is applied to them. Fortunately, bones are highly active organs that can repair themselves if they break. Bones can also remodel themselves and grow. You’ll learn how bones can do all of these things in this section.
Bone Growth
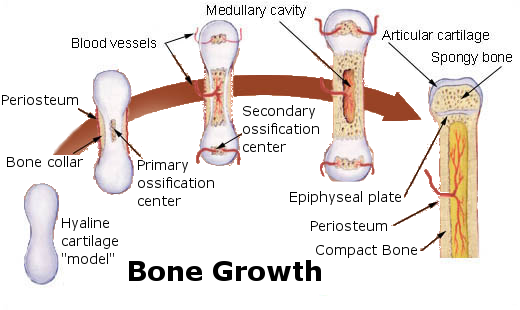
Early in the development of a human fetus, the skeleton is made almost entirely of cartilage. The relatively soft cartilage gradually turns into hard bone through ossification. Ossification is a process in which bone tissue is created from cartilage. The steps in which bones of the skeleton form from cartilage are illustrated in 11.5.2. The steps are as follows:
- Cartilage “model” of bone forms. This model continues to grow as ossification takes place.
- Ossification begins at a primary ossification center in the middle of bone.
- Ossification then starts to occur at secondary ossification centers at the ends of bone.
- The medullary cavity forms. This cavity will contain red bone marrow.
- Areas of ossification meet at epiphyseal plates, and articular cartilage forms. Bone growth ends.
The ossification of cartilage in the human skeleton is a process that lasts throughout childhood in some bones.
Primary and Secondary Ossification Centers
When bone forms from cartilage, ossification begins with a point in the cartilage called the primary ossification center. This generally appears during fetal development, although a few short bones begin their primary ossification after birth. Ossification happens toward both ends of the bone from the primary ossification center, and — in the case of long bones — it eventually forms the shaft of the bone.
Secondary ossification centers form after birth. Ossification from secondary centers eventually forms the ends of the bones. The shaft and ends of the bone are separated by a growing zone of cartilage until the individual reaches skeletal maturity.
Skeletal Maturity
Throughout childhood, the cartilage remaining in the skeleton keeps growing, and allows for bones to grow in size. Once all of the cartilage has been replaced by bone, and fusion has taken place at the epiphyseal plates, bones can no longer keep growing in length. At this point, skeletal maturity has been reached. It generally takes place by age 18 to 25.
The use of anabolic steroids by teens can speed up the process of skeletal maturity, resulting in a shorter period of cartilage growth before fusion takes place. This means that teens who use steroids are likely to end up shorter as adults than they would otherwise have been.
Bone Remodeling
Even after skeletal maturity has been attained, bone is constantly being resorbed and replaced with new bone in a process called bone remodeling. In this lifelong process, mature bone tissue is continually turned over, with about ten per cent of the skeletal mass of an adult being remodeled each year. Bone remodeling is carried out through the work of osteoclasts — which are bone cells that resorb bone and dissolve its minerals — and osteoblasts, which are bone cells that make new bone matrix.
Bone remodeling serves several functions. It shapes the bones of the skeleton as a child grows, and it repairs tiny flaws in bone that result from everyday movements. Remodeling also makes bones thicker at points where muscles place the most stress on them. In addition, remodeling helps regulate mineral homeostasis, because it either releases mineral from bones into the blood or absorbs mineral from the blood into bones. Figure 11.5.3 shows how osteoclasts in bones are involved in calcium regulation.
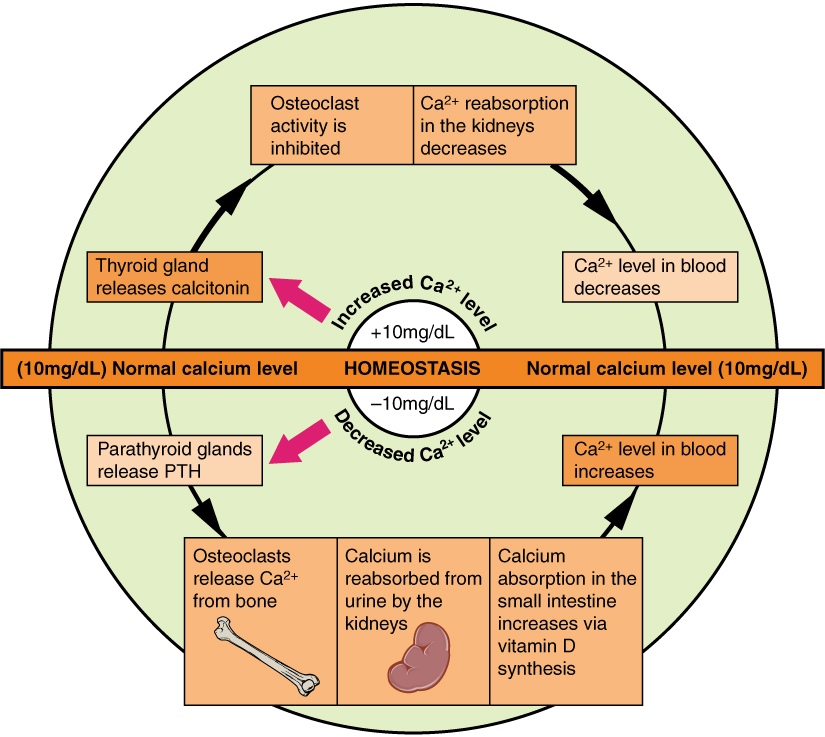
The action of osteoblasts and osteoclasts in bone remodeling and calcium homeostasis is controlled by a number of enzymes, hormones, and other substances that either promote or inhibit the activity of the cells. In this way, these substances control the rate at which bone is made, destroyed, and changed in shape. For example, the rate at which osteoclasts resorb bone and release calcium into the blood is promoted by parathyroid hormone (PTH) and inhibited by calcitonin, which is produced by the thyroid gland (see the diagram in Figure 11.5.3). The rate at which osteoblasts create new bone is stimulated by growth hormone, which is produced by the anterior lobe of the pituitary gland. Thyroid hormone and sex hormones (estrogens and androgens) also stimulate osteoblasts to create new bone.
Bone Repair
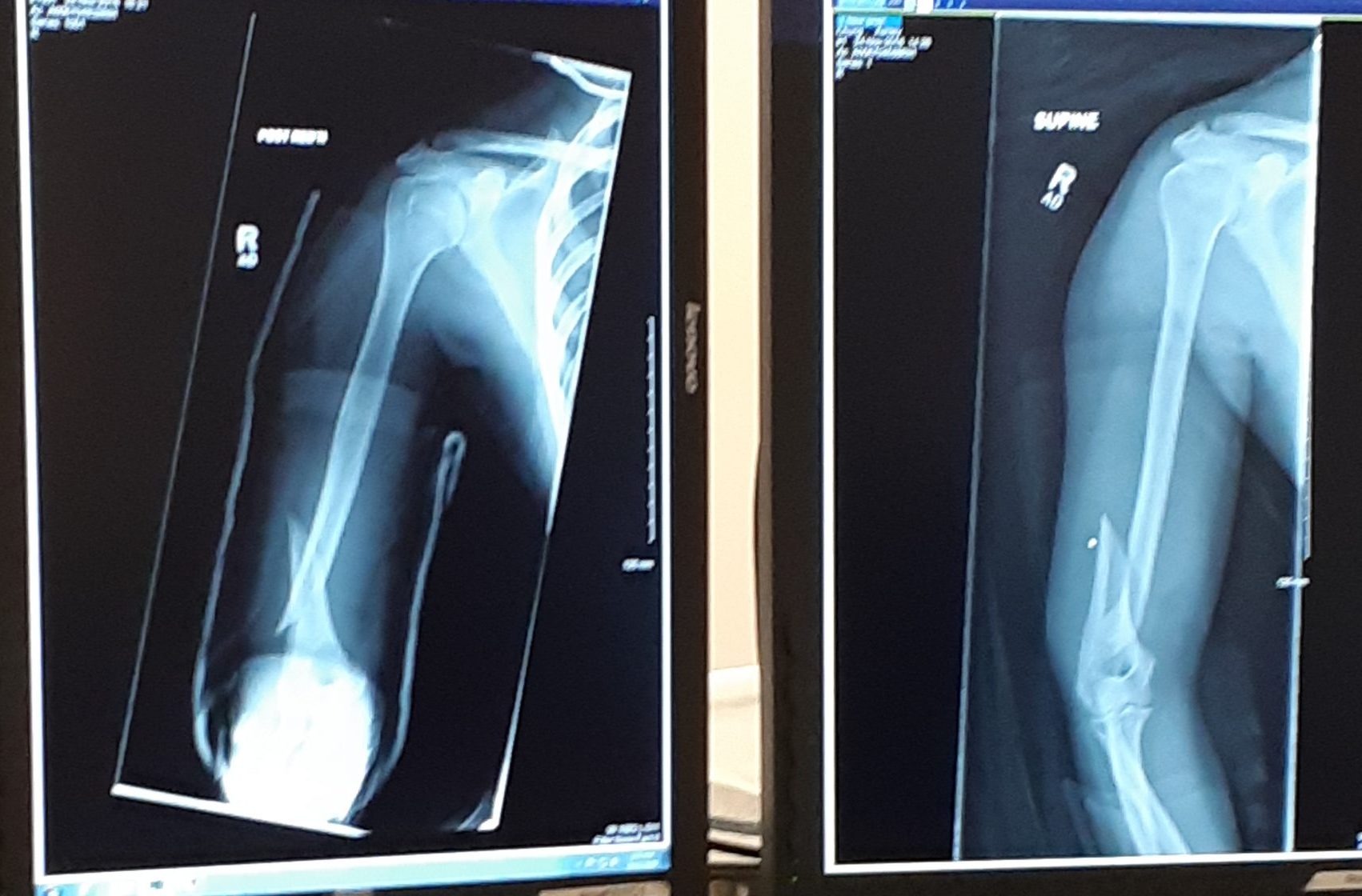
Bone repair (or healing) is the process in which a bone repairs itself following a bone fracture. You can see an X-ray of a bone fracture in Figure 11.5.4. In this fracture, the humerus in the upper arm has been completely broken through its shaft. Before this fracture heals, a physician must push the displaced bone parts back into their correct positions. Then, the bone must be stabilized — with a cast and/or pins surgically inserted into the bone, for example (as shown in Figure 11.5.5) — until the bone’s natural healing process is complete. This process may take several weeks.
 |
 |
Although bone repair is a natural physiological process, it may be promoted or inhibited by several factors. Fracture repair is more likely to be successful with adequate nutrient intake. Age, bone type, drug therapy, and pre-existing bone disease are additional factors that may affect healing. Bones that are weakened by disease (such as osteoporosis or bone cancer) are not only likely to heal more slowly, but are also more likely to fracture in the first place.
Feature: Myth vs. Reality
Bone fractures are fairly common, and there are many myths about them. Knowing the facts is important, because fractures generally require emergency medical treatment.
| Myth | Reality |
|---|---|
| “A bone fracture is a milder injury than a broken bone.” | A bone fracture is the same thing as a broken bone. |
| “If you still have full range of motion in a limb, then it must not be fractured.” | Even if a bone is fractured, the muscles and tendons attached to it may still be able to move the bone normally. This is especially likely if the bone is cracked — but not broken — into two pieces. Even if a bone is broken all the way through, range of motion may not be affected if the bones on either side of the fracture remain properly aligned. |
| “A fracture always produces a bruise.” | Many — but not all — fractures produce a bruise. If a fracture does produce a bruise, it may take several hours (or even a day or more!) for the bruise to appear. |
| “Fractures are so painful that you will immediately know if you break a bone.” | Ligament sprains and muscle strains are also very painful, sometimes more painful than fractures. Additionally, every person has a different pain tolerance. People with a high pain tolerance may continue using a broken bone in spite of the pain. |
| “You can tell when a bone is fractured because there will be very localized pain over the break.” | A broken bone is often accompanied by injuries to surrounding muscles or ligaments. As a result, the pain may extend far beyond the location of the fracture. The pain may be greater directly over the fracture, but the intensity of the pain may make it difficult to pinpoint exactly where the pain originates. |
11.5 Summary
- Bone is very active tissue. Its cells are constantly forming and resorbing bone matrix.
- Early in the development of a human fetus, the skeleton is made almost entirely of cartilage. The relatively soft cartilage gradually turns into hard bone. This is called ossification. It begins at a primary ossification center in the middle of bone, and later also occurs at secondary ossification centers in the ends of bone. The bone can no longer grow in length after the areas of ossification meet and fuse at the time of skeletal maturity.
- Throughout life, bone is constantly being replaced in the process of bone remodeling. In this process, osteoclasts resorb bone, and osteoblasts make new bone to replace it. Bone remodeling shapes the skeleton, repairs tiny flaws in bones, and helps maintain mineral homeostasis in the blood.
- Bone repair is the natural process in which a bone repairs itself following a bone fracture. This process may take several weeks. In the process, periosteum produces cells that develop into osteoblasts, and the osteoblasts form new bone matrix to heal the fracture. Bone repair may be affected by diet, age, pre-existing bone disease, or other factors.
11.5 Review Questions
- Outline how bone develops starting early in the fetal stage, and through the age of skeletal maturity.
- Describe the process of bone remodeling. When does it occur?
- What purposes does bone remodeling serve?
- Define bone repair. How long does this process take?
- Explain how bone repair occurs.
- Identify factors that may affect bone repair.
-
- If there is a large region between the primary and secondary ossification centers in a bone, is the person young or old? Explain your answer.
- If bones can repair themselves, why are casts and pins sometimes necessary in the process?
- When calcium levels are low, which type of bone cell causes the release of calcium to the bloodstream?
- Which tissue and bone cell type are primarily involved in bone repair after a fracture?
- Describe one way in which hormones are involved in bone remodeling.
11.5 Explore More
How to grow a bone – Nina Tandon, TED-Ed, 2015.
Healing Process of Bone Fracture, Aldo Fransiskus Marsetio, 2015.
The Skeleton From Fetal to Adult, Samantha Espolt, 2012.
Attributions
Figure 11.5.1
First_plaster_long_leg_cast…._-_9383569051 by 4x4king10 on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 11.5.2
Bone_growth by Chaldor (derivative work) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/en:Public_domain). (Original, Illu_bone_growth.jpg is by Fuelbottle)
Figure 11.5.3
Calcium_Homeostasis by OpenStax on Wikimedia commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0/deed.en) license.
Figure 11.5.4
Broken Arm by Ashley Chung is used with permission.
Figure 11.5.5
Broken Arm with plate and pins by Ashley Chung is used with permission.
References
Aldo Fransiskus Marsetio. (2015, ). Healing process of bone fracture. YouTube. https://www.youtube.com/watch?v=-P6LsendHxU
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 6.24 Pathways in calcium homeostasis [digital image]. In Anatomy and Physiology (Section 6.7). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/6-7-calcium-homeostasis-interactions-of-the-skeletal-system-and-other-organ-systems
Samantha Espolt. (2012, ). The skeleton from fetal to adult. YouTube. https://www.youtube.com/watch?v=RC2w_9DcY38&t=3s
TED-Ed. (2015, ). How to grow a bone – Nina Tandon. YouTube. https://www.youtube.com/watch?v=yJoQj5-TIvE
The process in which cartilage is changed into bone.
The first area of a bone to start ossifying. It usually appears during prenatal development in the central part of each developing bone. In long bones the primary centers occur in the diaphysis/shaft and in irregular bones the primary centers occur usually in the body of the bone.
The area of ossification that appears after the primary ossification center has already appeared – most of which appear during the postnatal and adolescent years. Most bones have more than one secondary ossification center. In long bones, the secondary centers appear in the epiphyses.
Supportive connective tissue that provides a smooth surface for the movement of bones at joints. Contains cells called chondrocytes.
Also known as the growth plate, a thin layer of cartilage that lies between the epiphyses and metaphyses, where the growth of long bones takes place.
A synthetic steroid hormone that resembles testosterone in promoting the growth of muscle. Such hormones are used medicinally to treat some forms of weight loss and (illegally) by some athletes and others to enhance physical performance.
The continuous, lifelong process in which existing bone is resorbed by osteoclasts and new bone is made by osteoblasts.
A type of bone cell that breaks down bone, dissolves its minerals, and releases them into the blood.
A type of bone cell that makes and mineralizes bone matrix.
The ability of an organism to maintain constant internal conditions despite external changes.
Biological molecules that lower amount the energy required for a reaction to occur.
A hormone is a signaling molecule produced by glands in multicellular organisms that target distant organs to regulate physiology and behavior.
A hormone secreted by the parathyroid gland which helps regulate blood calcium.
A large endocrine gland in the neck whose hormones control the rate of cellular metabolism and help maintain calcium homeostasis.
The process in which bone heals itself following a bone fracture.
A rigid organ that constitutes part of the vertebrate skeleton in animals.
A tough, fibrous membrane that covers the outer surface of bones.

