16.4 Kidneys
Created by CK-12 Foundation/Adapted by Christine Miller

Kidneys on the Menu
Pictured in Figure 16.4.1 is a steak and kidney pie; this savory dish is a British favorite. When kidneys are on a menu, they typically come from sheep, pigs, or cows. In these animals (as in the human animal), kidneys are the main organs of excretion.
Location of the Kidneys
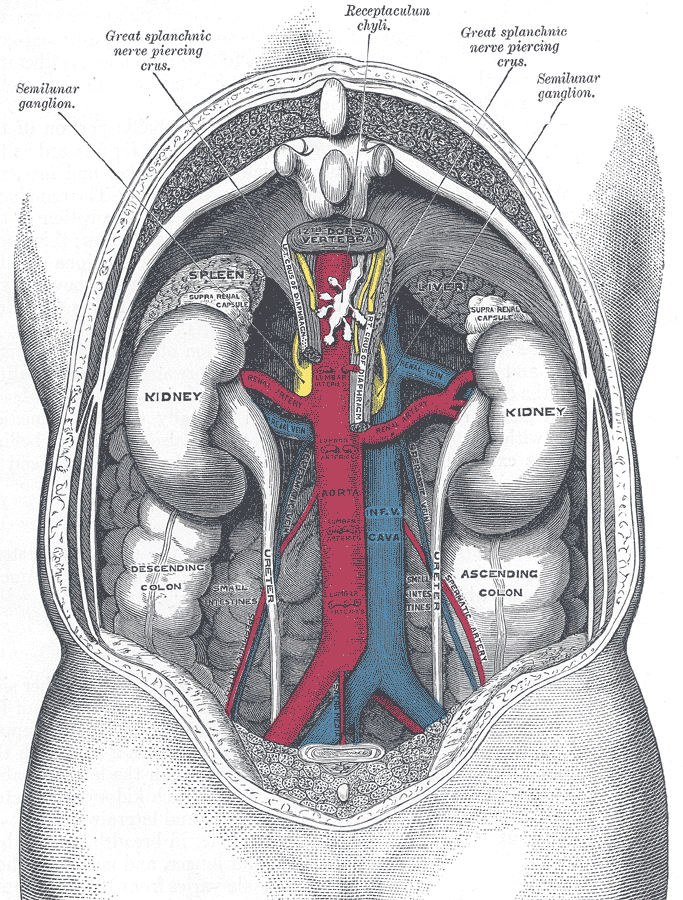
The two bean-shaped kidneys are located high in the back of the abdominal cavity, one on each side of the spine. Both kidneys sit just below the diaphragm, the large breathing muscle that separates the abdominal and thoracic cavities. As you can see in the following figure, the right kidney is slightly smaller and lower than the left kidney. The right kidney is behind the liver, and the left kidney is behind the spleen. The location of the liver explains why the right kidney is smaller and lower than the left.
Kidney Anatomy
The shape of each kidney gives it a convex side (curving outward) and a concave side (curving inward). You can see this clearly in the detailed diagram of kidney anatomy shown in Figure 16.4.3. The concave side is where the renal artery enters the kidney, as well as where the renal vein and ureter leave the kidney. This area of the kidney is called the hilum. The entire kidney is surrounded by tough fibrous tissue — called the renal capsule — which, in turn, is surrounded by two layers of protective, cushioning fat.
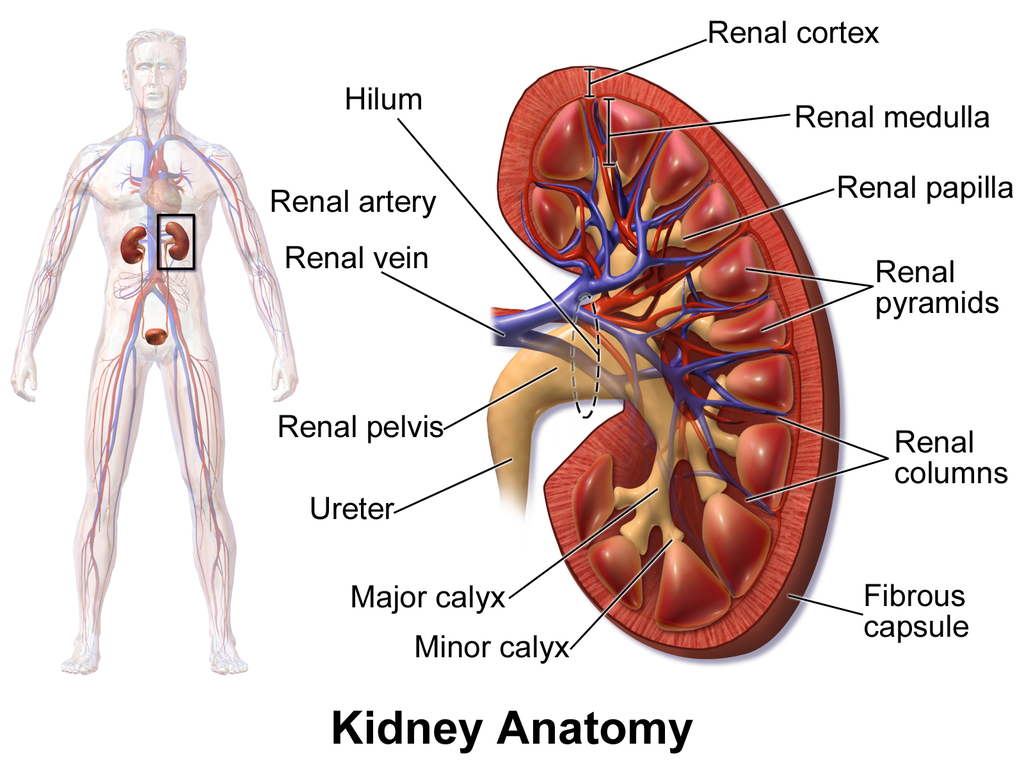
Internally, each kidney is divided into two major layers: the outer renal cortex and the inner renal medulla (see Figure 16.4.3 above). These layers take the shape of many cone-shaped renal lobules, each containing renal cortex surrounding a portion of medulla called a renal pyramid. Within the renal pyramids are the structural and functional units of the kidneys, the tiny nephrons. Between the renal pyramids are projections of cortex called renal columns. The tip, or papilla, of each pyramid empties urine into a minor calyx (chamber). Several minor calyces empty into a major calyx, and the latter empty into the funnel-shaped cavity called the renal pelvis, which becomes the ureter as it leaves the kidney.
Renal Circulation
The renal circulation is an important part of the kidney’s primary function of filtering waste products from the blood. Blood is supplied to the kidneys via the renal arteries. The right renal artery supplies the right kidney, and the left renal artery supplies the left kidney. These two arteries branch directly from the aorta, which is the largest artery in the body. Each kidney is only about 11 cm (4.4 in) long, and has a mass of just 150 grams (5.3 oz), yet it receives about ten per cent of the total output of blood from the heart. Blood is filtered through the kidneys every 3 minutes, 24 hours a day, every day of your life.
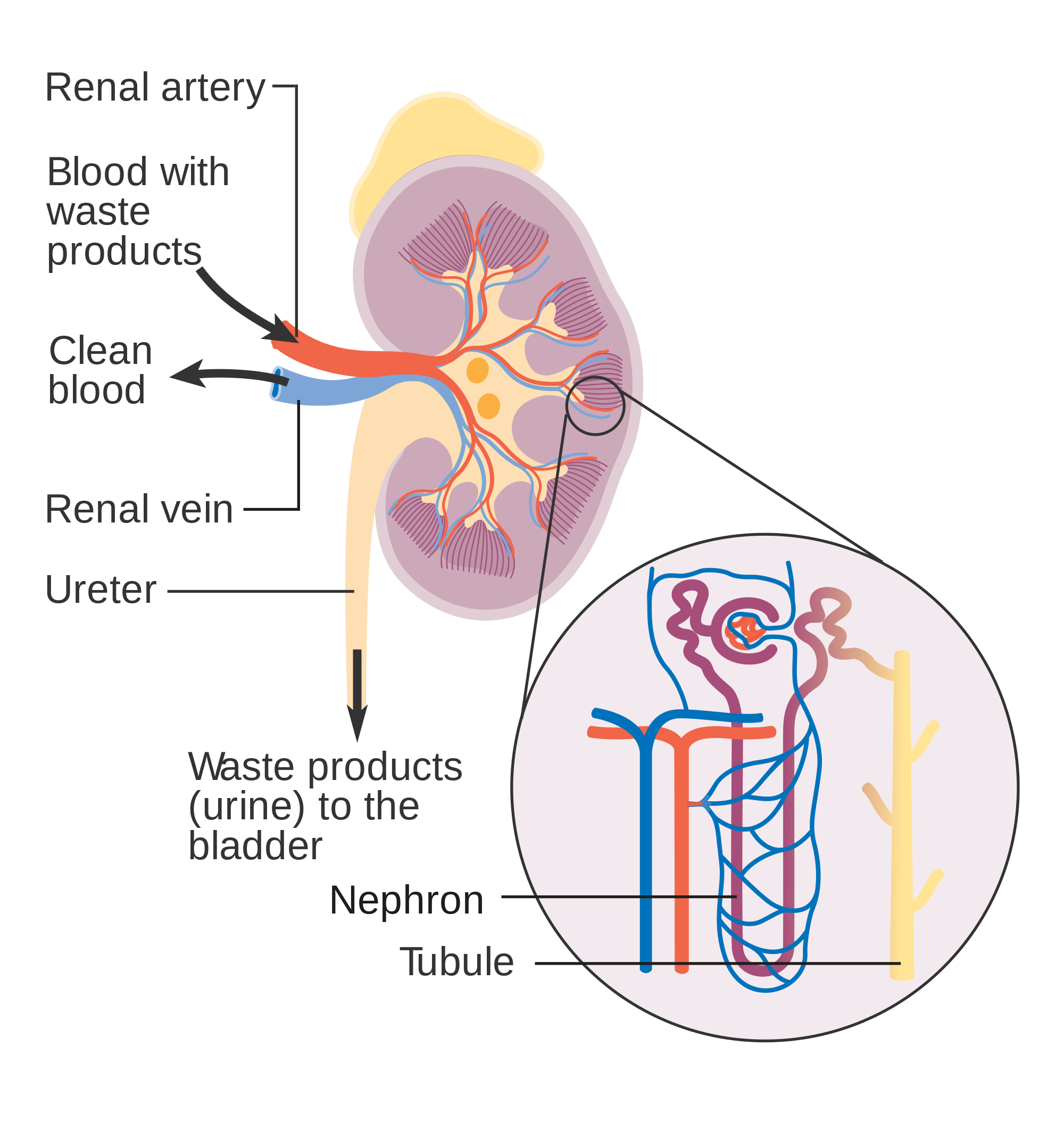
As indicated in Figure 16.4.4, each renal artery carries blood with waste products into the kidney. Within the kidney, the renal artery branches into increasingly smaller arteries that extend through the renal columns between the renal pyramids. These arteries, in turn, branch into arterioles that penetrate the renal pyramids. Blood in the arterioles passes through nephrons, the structures that actually filter the blood. After blood passes through the nephrons and is filtered, the clean blood moves through a network of venules that converge into small veins. Small veins merge into increasingly larger ones, and ultimately into the renal vein, which carries clean blood away from the kidney to the inferior vena cava.
Nephron Structure and Function
Figure 16.4.4 gives an indication of the complex structure of a nephron. The nephron is the basic structural and functional unit of the kidney, and each kidney typically contains at least a million of them. As blood flows through a nephron, many materials are filtered out of the blood, needed materials are returned to the blood, and the remaining materials form urine. Most of the waste products removed from the blood and excreted in urine are byproducts of metabolism. At least half of the waste is urea, a waste product produced by protein catabolism. Another important waste is uric acid, produced in nucleic acid catabolism.
Components of a Nephron
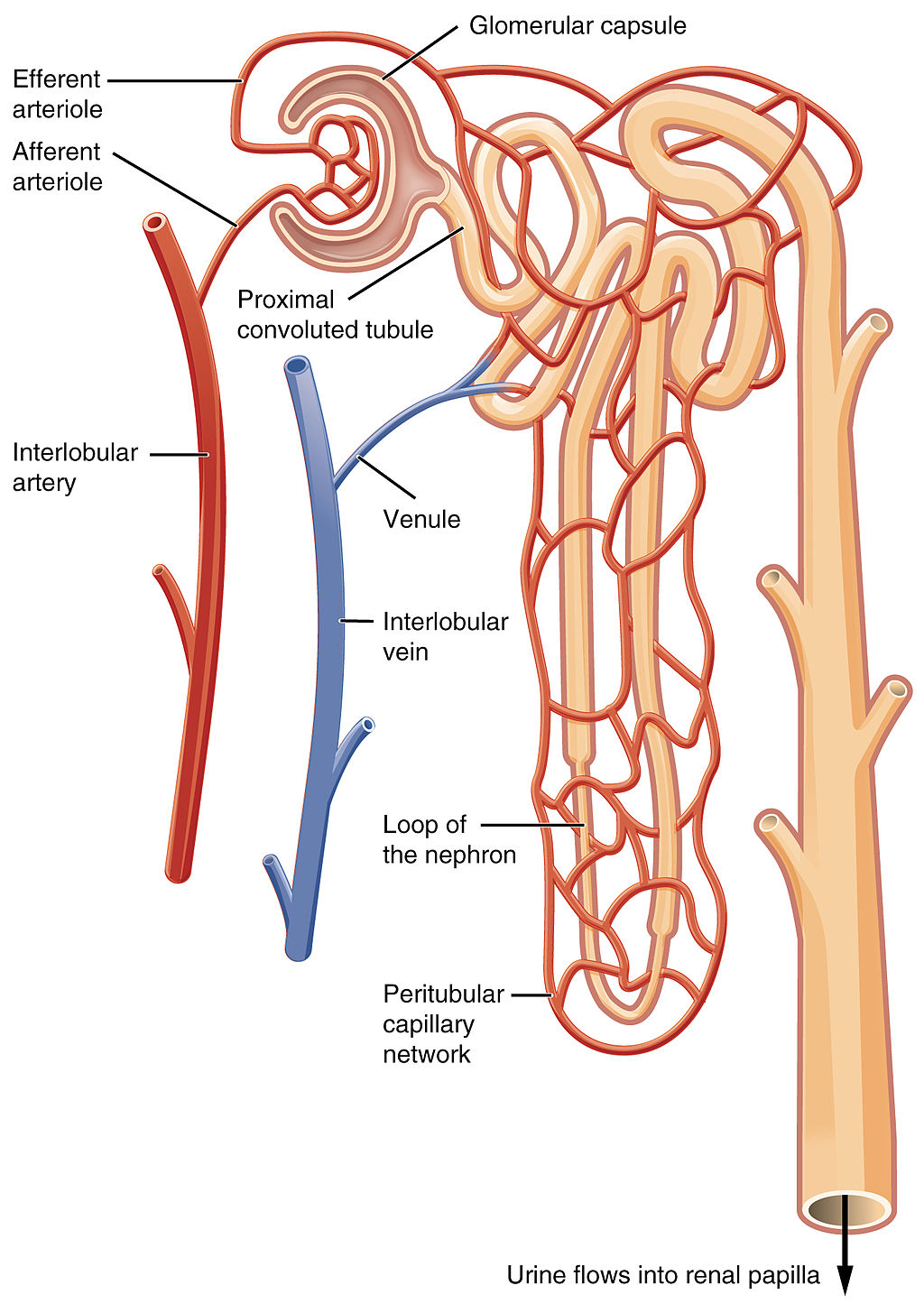
Figure 16.4.5 shows in greater detail the components of a nephron. Each nephron is composed of an initial filtering component that consists of a network of capillaries called the glomerulus (plural, glomeruli), which is surrounded by a space within a structure called glomerular capsule (also known as the Bowman’s capsule). Extending from glomerular capsule is the renal tubule. The proximal end (nearest glomerular capsule) of the renal tubule is called the proximal convoluted (coiled) tubule. From here, the renal tubule continues as a loop (known as the loop of Henle) (also known as the loop of the nephron), which in turn becomes the distal convoluted tubule. The latter finally joins with a collecting duct. As you can see in the diagram, arterioles surround the total length of the renal tubule in a mesh called the peritubular capillary network.
Function of a Nephron
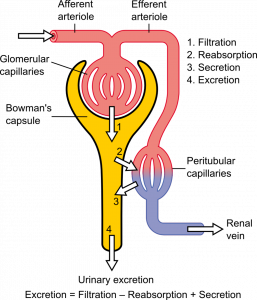
The simplified diagram of a nephron in Figure 16.4.6 shows an overview of how the nephron functions. Blood enters the nephron through an arteriole called the afferent arteriole. Next, some of the blood passes through the capillaries of the glomerulus. Any blood that doesn’t pass through the glomerulus — as well as blood after it passes through the glomerular capillaries — continues on through an arteriole called the efferent arteriole. The efferent arteriole follows the renal tubule of the nephron, where it continues playing a role in nephron functioning.
Filtration
As blood from the afferent arteriole flows through the glomerular capillaries, it is under pressure. Because of the pressure, water and solutes are filtered out of the blood and into the space made by glomerular capsule, almost like the water you cook pasta is is filtered out through a strainer. This is the filtration stage of nephron function. The filtered substances — called filtrate — pass into glomerular capsule, and from there into the proximal end of the renal tubule. Anything too large to move through the pores in the glomerulus, such as blood cells, large proteins, etc., stay in the cardiovascular system. At this stage, filtrate (fluid in the nephron) includes water, salts, organic solids (such as nutrients), and waste products of metabolism (such as urea).
Reabsorption and Secretion
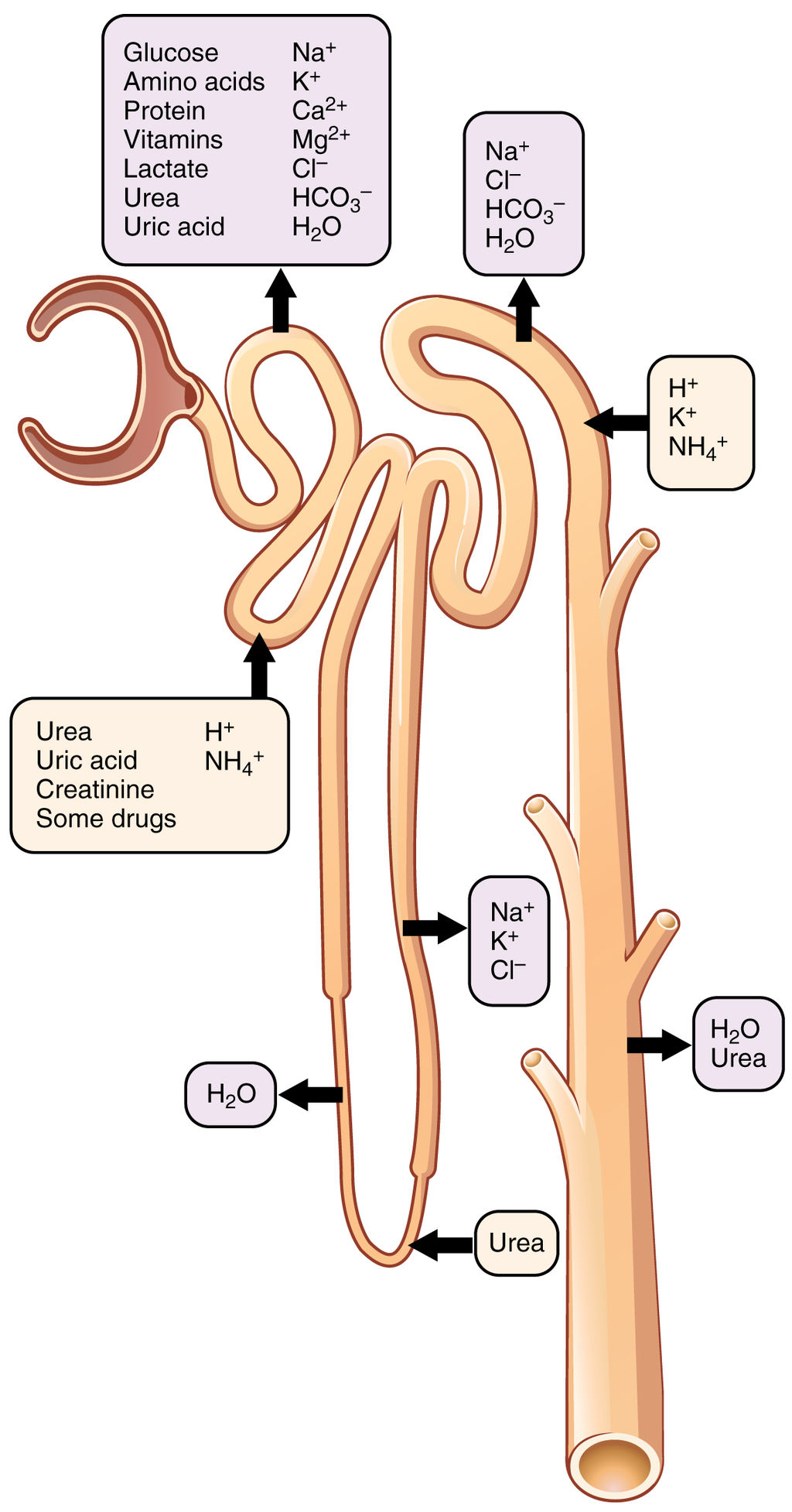
As filtrate moves through the renal tubule, some of the substances it contains are reabsorbed from the filtrate back into the blood in the efferent arteriole (via peritubular capillary network). This is the reabsorption stage of nephron function and it is about returning “the good stuff” back to the blood so that it doesn’t exit the body in urine. About two-thirds of the filtered salts and water, and all of the filtered organic solutes (mainly glucose and amino acids) are reabsorbed from the filtrate by the blood in the peritubular capillary network. Reabsorption occurs mainly in the proximal convoluted tubule and the loop of Henle, as seen in Figure 16.4.7.
At the distal end of the renal tubule, some additional reabsorption generally occurs. This is also the region of the tubule where other substances from the blood are added to the filtrate in the tubule. The addition of other substances to the filtrate from the blood is called secretion. Both reabsorption and secretion (shown in Figure 16.4.7) in the distal convoluted tubule are largely under the control of endocrine hormones that maintain homeostasis of water and mineral salts in the blood. These hormones work by controlling what is reabsorbed into the blood from the filtrate and what is secreted from the blood into the filtrate to become urine. For example, parathyroid hormone causes more calcium to be reabsorbed into the blood and more phosphorus to be secreted into the filtrate.
Collection of Urine and Excretion

By the time the filtrate has passed through the entire renal tubule, it has become the liquid waste known as urine. Urine empties from the distal end of the renal tubule into a collecting duct. From there, the urine flows into increasingly larger collecting ducts. As urine flows through the system of collecting ducts, more water may be reabsorbed from it. This will occur in the presence of antidiuretic hormone from the posterior pituitary gland. This hormone makes the collecting ducts permeable to water, allowing water molecules to pass through them into capillaries by osmosis, while preventing the passage of ions or other solutes. As much as 75% of the water may be reabsorbed from urine in the collecting ducts, making the urine more concentrated.
Urine finally exits the largest collecting ducts through the renal papillae. It empties into the renal calyces, and finally into the renal pelvis. From there, it travels through the ureter to the urinary bladder for eventual excretion from the body. An average of roughly 1.5 litres (a little over 6 cups) of urine is excreted each day. Normally, urine is yellow or amber in colour (see Figure 16.4.8). The darker the colour, generally speaking, the more concentrated the urine is.
Besides filtering blood and forming urine for excretion of soluble wastes, the kidneys have several vital functions in maintaining body-wide homeostasis. Most of these functions are related to the composition or volume of urine formed by the kidneys. The kidneys must maintain the proper balance of water and salts in the body, normal blood pressure, and the correct range of blood pH. Through the processes of absorption and secretion by nephrons, more or less water, salt ions, acids, or bases are returned to the blood or excreted in urine, as needed, to maintain homeostasis.
Blood Pressure Regulation
The kidneys do not control homeostasis all alone. As indicated above, endocrine hormones are also involved. Consider the regulation of blood pressure by the kidneys. Blood pressure is the pressure exerted by blood on the walls of the arteries. The regulation of blood pressure is part of a complex system, called the renin-angiotensin-aldosterone system. This system regulates the concentration of sodium in the blood to control blood pressure.
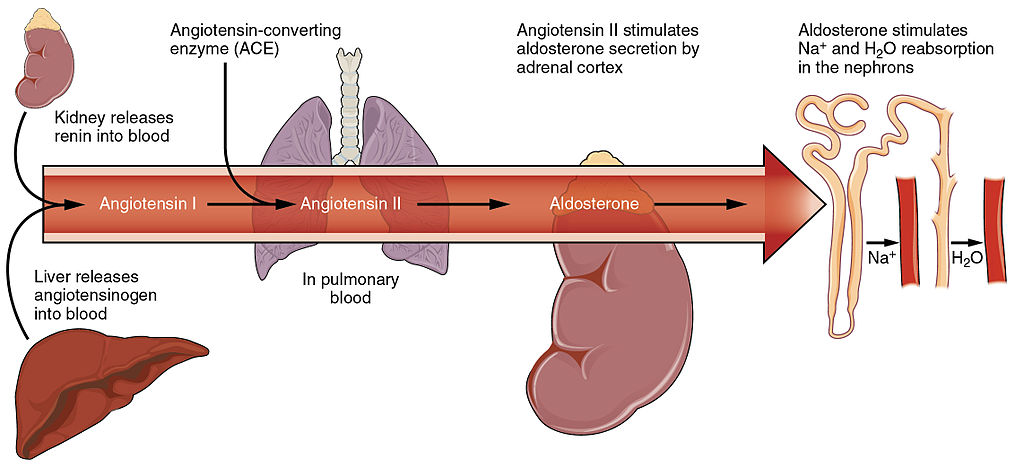
The renin-angiotensin-aldosterone system is put into play when the concentration of sodium ions in the blood falls lower than normal. This causes the kidneys to secrete an enzyme called renin into the blood. It also causes the liver to secrete a protein called angiotensinogen. Renin changes angiotensinogen into a proto-hormone called angiotensin I. This is converted to angiotensin II by an enzyme (angiotensin-converting enzyme) in lung capillaries.
Angiotensin II is a potent hormone that causes arterioles to constrict. This, in turn, increases blood pressure. Angiotensin II also stimulates the secretion of the hormone aldosterone from the adrenal cortex. Aldosterone causes the kidneys to increase the reabsorption of sodium ions and water from the filtrate into the blood. This returns the concentration of sodium ions in the blood to normal. The increased water in the blood also increases blood volume and blood pressure.
Other Kidney Hormones
Hormones other than renin are also produced and secreted by the kidneys. These include calcitriol and erythropoietin.
- Calcitriol is secreted by the kidneys in response to low levels of calcium in the blood. This hormone stimulates uptake of calcium by the intestine, thus raising blood levels of calcium.
- Erythropoietin is secreted by the kidneys in response to low levels of oxygen in the blood. This hormone stimulates erythropoiesis, which is the production of erythrocytes in bone marrow. Extra red blood cells increase the level of oxygen carried in the blood.
Feature: Human Biology in the News
Kidney failure is a complication of common disorders including diabetes mellitus and hypertension. It is estimated that approximately 12.5% of Canadians have some form of kidney disease. If the disease is serious, the patient must either receive a donated kidney or have frequent hemodialysis, a medical procedure in which the blood is artificially filtered through a machine. Transplant generally results in better outcomes than hemodialysis, but demand for organs far outstrips the supply. The average time on the organ donation waitlist for a kidney is four years. There are over 3,000 Canadians on the wait list for a kidney transplant and some will die waiting for a kidney to become available.
For the past decade, Dr. William Fissell, a kidney specialist at Vanderbilt University, has been working to create an implantable part-biological and part-artificial kidney. Using microchips like those used in computers, he has produced an artificial kidney small enough to implant in the patient’s body in place of the failed kidney. According to Dr. Fissell, the artificial kidney is “… a bio-hybrid device that can mimic a kidney to remove enough waste products, salt, and water to keep a patient off [hemo]dialysis.”
The filtration system in the artificial kidney consists of a stack of 15 microchips. Tiny pores in the microchips act as a scaffold for the growth of living kidney cells that can mimic the natural functions of the kidney. The living cells form a membrane to filter the patient’s blood as a biological kidney would, but with less risk of rejection by the patient’s immune system, because they are embedded within the device. The new kidney doesn’t need a power source, because it uses the natural pressure of blood flowing through arteries to push the blood through the filtration system. A major part of the design of the artificial organ was devoted to fine tuning the fluid dynamics so blood flows through the device without clotting.
Because of the potential life-saving benefits of the device, the implantable kidney was given fast-track approval for testing in people by the U.S. Food and Drug Administration. The artificial kidney is expected to be tested in pilot trials by 2018. Dr. Fissell says he has a long list of patients eager to volunteer for the trials.
16.4 Summary
- The two bean-shaped kidneys are located high in the back of the abdominal cavity on either side of the spine. A renal artery connects each kidney with the aorta, and transports unfiltered blood to the kidney. A renal vein connects each kidney with the inferior vena cava and transports filtered blood back to the circulation.
- The kidney has two main layers involved in the filtration of blood and formation of urine: the outer cortex and inner medulla. At least a million nephrons — which are the tiny functional units of the kidney — span the cortex and medulla. The entire kidney is surrounded by a fibrous capsule and protective fat layers.
- As blood flows through a nephron, many materials are filtered out of the blood, needed materials are returned to the blood, and the remaining materials are used to form urine.
- In each nephron, the glomerulus and surrounding Bowman’s capsule form the unit that filters blood. From Bowman’s capsule, the material filtered from blood (called filtrate) passes through the long renal tubule. As it does, some substances are reabsorbed into the blood, and other substances are secreted from the blood into the filtrate, finally forming urine. The urine empties into collecting ducts, where more water may be reabsorbed.
- The kidneys control homeostasis with the help of endocrine hormones. The kidneys, for example, are part of the renin-angiotensin-aldosterone system that regulates the concentration of sodium in the blood to control blood pressure. In this system, the enzyme renin secreted by the kidneys works with hormones from the liver and adrenal gland to stimulate nephrons to reabsorb more sodium and water from urine.
- The kidneys also secrete endocrine hormones, including calcitriol — which helps control the level of calcium in the blood — and erythropoietin, which stimulates bone marrow to produce red blood cells.
16.4 Review Questions
-
- Contrast the renal artery and renal vein.
- Identify the functions of a nephron. Describe in detail what happens to fluids (blood, filtrate, and urine) as they pass through the parts of a nephron.
- Identify two endocrine hormones secreted by the kidneys, along with the functions they control.
- Name two regions in the kidney where water is reabsorbed.
- Is the blood in the glomerular capillaries more or less filtered than the blood in the peritubular capillaries? Explain your answer.
- What do you think would happen if blood flow to the kidneys is blocked?
16.4 Explore More
How do your kidneys work? – Emma Bryce, TED-Ed, 2015.
https://youtu.be/es-t8lO1KpA
Urine Formation, Hamada Abass, 2013.
Printing a human kidney – Anthony Atala, TED-Ed, 2013.
Attributions
Figure 16.4.1
Steak and Kidney Pie by Charles Haynes on Flickr is used under a CC BY-SA 2.0 (https://creativecommons.org/licenses/by-sa/2.0/) license.
Figure 16.4.2
Gray Kidneys by Henry Vandyke Carter (1831-1897) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/public_domain). (Bartleby.com: Gray’s Anatomy, Plate 1120).
Figure 16.4.3
Blausen_0592_KidneyAnatomy_01 by BruceBlaus on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.4
Diagram_showing_how_the_kidneys_work_CRUK_138.svg by Cancer Research UK on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 16.4.5
Blood_Flow_in_the_Nephron by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.6
1024px-Physiology_of_Nephron by Madhero88 on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.7
Nephron_Secretion_Reabsorption by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
Figure 16.4.8
Urine by User:Markhamilton at English Wikipedia on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 16.4.9
Renin_Angiotensin_System-01 by OpenStax College on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
References
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 25.10 Blood flow in the nephron [digital image]. In Anatomy and Physiology (Section 25.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/25-3-gross-anatomy-of-the-kidney
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 25.17 Locations of secretion and reabsorption in the nephron [digital image]. In Anatomy and Physiology (Section 25.6). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/25-6-tubular-reabsorption
Betts, J. G., Young, K.A., Wise, J.A., Johnson, E., Poe, B., Kruse, D.H., Korol, O., Johnson, J.E., Womble, M., DeSaix, P. (2013, June 19). Figure 26.14 The renin-angiotensin system [digital image]. In Anatomy and Physiology (Section 26.3). OpenStax. https://openstax.org/books/anatomy-and-physiology/pages/26-3-electrolyte-balance
Blausen.com Staff. (2014). Medical gallery of Blausen Medical 2014. WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436
Hamada Abass. (2013). Urine formation. YouTube. https://www.youtube.com/watch?v=es-t8lO1KpA&feature=youtu.be
TED-Ed. (2015, February 9). How do your kidneys work? – Emma Bryce. YouTube. https://www.youtube.com/watch?v=FN3MFhYPWWo&feature=youtu.be
TED-Ed. (2013, March 15). Printing a human kidney – Anthony Atala. YouTube. https://www.youtube.com/watch?v=bX3C201O4MA&feature=youtu.be
One of a pair of organs of the excretory and urinary systems that filters wastes and excess water out of blood and forms urine.
A large cavity found in the torso of mammals between the thoracic cavity, which it is separated from by the thoracic diaphragm, and the pelvic cavity. Organs of the abdominal cavity include the stomach, liver, gallbladder, spleen, pancreas, small intestine, kidneys, large intestine, and adrenal glands.
A large, dome-shaped muscle below the lungs that allows breathing to occur when it alternately contracts and relaxes.
An organ of digestion and excretion that secretes bile for lipid digestion and breaks down excess amino acids and toxins in the blood.
A secondary organ of the lymphatic system where blood and lymph are filtered.
The entry and exit site for structures servicing the kidneys: vessels, nerves, lymphatics, and ureters.
A thin membranous sheath that covers the outer surface of each kidney. The capsule is composed of tough fibres, chiefly collagen and elastin (fibrous proteins), that help to support the kidney mass and protect the vital tissue from injury.
The outer portion of the kidney between the renal capsule and the renal medulla.
The innermost part of the kidney. The renal medulla is split up into a number of sections, known as the renal pyramids.
Any of the triangular sections of tissue that constitute the medulla, or inner substance, of the kidney. The pyramids consist mainly of tubules that transport urine from the cortical, or outer, part of the kidney, where urine is produced, to the calyces, or cup-shaped cavities in which urine collects before it passes through the ureter to the bladder.
One of the million tiny structural and functional units of the kidney that filters blood and forms urine.
An extension of the renal cortex in between the renal pyramids. It allows the cortex to be better anchored. Each column consists of lines of blood vessels and urinary tubes and a fibrous material.
The funnel-like end of a ureter where it enters the kidney and where urine collects before it is transported through the ureter.
A body fluid in humans and other animals that delivers necessary substances such as nutrients and oxygen to the cells and transports metabolic waste products away from those same cells. In vertebrates, it is composed of blood cells suspended in blood plasma.
A type of blood vessel that carries blood away from the heart and toward the lungs or body.
A type of blood vessel that carries blood toward the heart from the lungs or body.
A large vein carrying deoxygenated blood into the heart. There are two in humans, the inferior vena cava (carrying blood from the lower body) and the superior vena cava (carrying blood from the head, arms, and upper body).
The chemical processes that occur in a living organism to sustain life.
Waste product of protein catabolism that is mainly filtered from blood in the kidneys and excreted in urine.
A class of biological molecule consisting of linked monomers of amino acids and which are the most versatile macromolecules in living systems and serve crucial functions in essentially all biological processes.
The breakdown of larger molecules into smaller ones.
A waste product of nucleic acid catabolism that is mainly filtered from blood by the kidneys and excreted in urine.
Large biomolecules, essential to all known forms of life. The term nucleic acid is the overall name for DNA and RNA. They are composed of nucleotides, which are the monomers made of three components: a 5-carbon sugar, a phosphate group and a nitrogenous base.
A network of capillaries in the nephron of a kidney where substances are filtered out of the blood.
A structure surrounding the glomerulus of a nephron in a kidney, also known as the Bowman's capsule, into which substances that are filtered out of blood are passed to the renal tubule.
A tubular structure of a nephron in a kidney through which filtered substances pass and where some filtered substances are reabsorbed by the blood and additional substances are secreted from the blood.
The portion of the nephron that lies between the glomerular capsule and the loop of Henle and functions especially in the resorption of sugar, sodium and chloride ions, and water from the glomerular filtrate.
The part of a kidney tubule which forms a long loop in the medulla of the kidney, from which water and salts are resorbed into the blood.
A portion of kidney nephron between the loop of Henle and the collecting tubule. It is the part of the nephron and that is concerned especially with the concentration of urine.
Tiny blood vessels, supplied by the efferent arteriole, that travel alongside nephrons allowing reabsorption and secretion between blood and the inner lumen of the nephron.
The fluid filtered from blood, called filtrate, passes through the nephron, much of the filtrate and its contents are reabsorbed into the body.
Glucose (also called dextrose) is a simple sugar with the molecular formula C6H12O6. Glucose is the most abundant monosaccharide, a subcategory of carbohydrates. Glucose is mainly made by plants and most algae during photosynthesis from water and carbon dioxide, using energy from sunlight.
Amino acids are organic compounds that combine to form proteins.
The process by which the nephron removes water and solutes from the tubular fluid (pre-urine) and returns them to the circulating blood.
Transport which occurs in the proximal tubule section of the nephron, and is responsible for the movement of certain molecules out of the blood and into the urine.
The ability of an organism to maintain constant internal conditions despite external changes.
A hormone secreted by the parathyroid gland which helps regulate blood calcium.
A liquid waste product of the body that is formed by the kidneys and excreted by the other organs of the urinary system.
One of a network of ducts in a kidney where additional water may be reabsorbed from urine.
also called vasopressin. A hormone made by the hypothalamus in the brain and stored in the posterior pituitary gland. It tells your kidneys how much water to conserve. ADH constantly regulates and balances the amount of water in your blood.
The master gland of the endocrine system that secretes many hormones, the majority of which regulate other endocrine glands.
The movement of water or other solvent through a plasma membrane from a region of low solute concentration to a region of high solute concentration.
A muscular, tube-like organ of the urinary system that moves urine by peristalsis from a kidney to the bladder.
A sac-like organ that stores urine until it is excreted from the body.
The measure of the force exerted by circulating blood on the walls of arteries.
A measure of the acidity or basicity of aqueous or other liquid solutions. The term translates the values of the concentration of the hydrogen ion in a scale ranging from 0 and 14. In pure water, which is neutral (neither acidic nor alkaline), the concentration of the hydrogen ion corresponds to a pH of 7. A solution with a pH less than 7 is considered acidic; a solution with a pH greater than 7 is considered basic, or alkaline.
An enzyme secreted by and stored in the kidneys which promotes the production of the protein angiotensin.
The active form of vitamin D, normally made in the kidney. A manufactured form is used to treat kidney disease with low blood calcium, hyperparathyroidism due to kidney disease, low blood calcium due to hypoparathyroidism, osteoporosis, osteomalacia, and familial hypophosphatemia.
A hormone secreted by the kidneys that increases the rate of production of red blood cells in response to falling levels of oxygen in the tissues.
A red blood cell that (in humans) is typically a biconcave disc without a nucleus. Erythrocytes contain the pigment hemoglobin, which imparts the red color to blood, and transport oxygen and carbon dioxide to and from the tissues.
A disorder in which blood sugar (glucose) levels are abnormally high because the body does not produce enough insulin to meet its needs.
A persistently high blood pressure, generally defined as 140/90 mm Hg or higher.

