17.5 Adaptive Immune System
Created by CK-12 Foundation/Adapted by Christine Miller
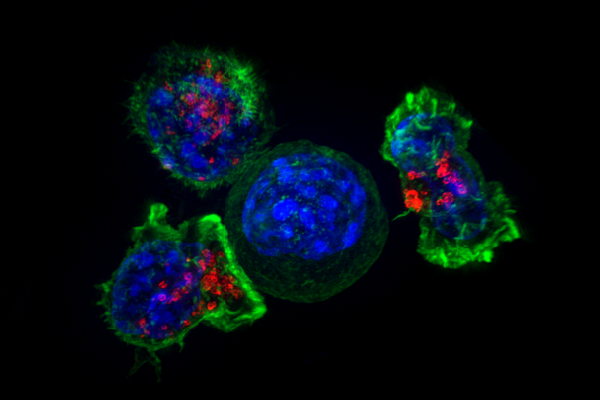
The Kiss of Death
The photomicrograph in Figure 17.5.1 shows a group of killer T cells (green and red) surrounding a cancer cell (blue, centre). When a killer T cell makes contact with the cancer cell, it attaches to and spreads over the dangerous target. The killer T cell then uses special chemicals stored in vesicles (red) to deliver the killing blow. This event has thus been nicknamed “the kiss of death.” After the target cell is killed, the killer T cells move on to find the next victim. Killer T cells like these are important players in the adaptive immune system.
What Is the Adaptive Immune System?
The adaptive immune system is a subsystem of the overall immune system. It is composed of highly specialized cells and processes that eliminate specific pathogens and tumor cells. An adaptive immune response is set in motion by antigens that the immune system recognizes as foreign. Unlike an innate immune response, an adaptive immune response is highly specific to a particular pathogen (or its antigen). An important function of the adaptive immune system that is not shared by the innate immune system is the creation of immunological memory — or immunity — which occurs after the initial response to a specific pathogen. It allows for a faster, stronger response on subsequent encounters with the same pathogen, usually before the pathogen can even cause symptoms of illness.
Lymphocytes are the main cells of the adaptive immune system. They are leukocytes that arise and mature in organs of the lymphatic system, including the bone marrow and thymus. The human body normally has about 2 trillion lymphocytes, which constitute about 1/3 of all leukocytes. Most of the lymphocytes are normally sequestered within tissue fluid or organs of the lymphatic system, including the tonsils, spleen, and lymph nodes. Only about 2% of the lymphocytes are normally circulating in the blood. There are two main types of lymphocytes involved in adaptive immune responses, called T cells and B cells. T cells destroy infected cells or release chemicals that regulate immune responses. B cells secrete antibodies that bind with antigens[/pb_glossary] of [pb_glossary id="271"]pathogens so they can be removed by other immune cells or processes.
Pathways of the Adaptive Immune Response
There are some general similarities in the way in which the separate adaptive immune responses occur in T cell and B cell responses. In both pathways, a foreign antigen is recognized by the B or T cell. From there, cytokines produced by helper T-cells promote clonal expansion of lymphocytes. From this clonal expansion, two types of B or T cells are produced- cells that directly fight the pathogen invasion and cells that remain behind to provide long-term immunity. Finally, once the pathogen invasion has been eradicated, the cells that provide the short-term response (called plasma cells and cytotoxic T-cells) go through apoptosis (programmed cell death). Only a few B and T cells, called memory cells, remain in the body to quickly activate a response in the antigen is encountered again.
T Cells
There are multiple types of T cells, or T lymphocytes. Major types are killer (or cytotoxic) T cells and helper T cells. Both types develop from immature T cells that become activated by exposure to an antigen.
T Cell Activation (or Cell-Mediated Immunity)
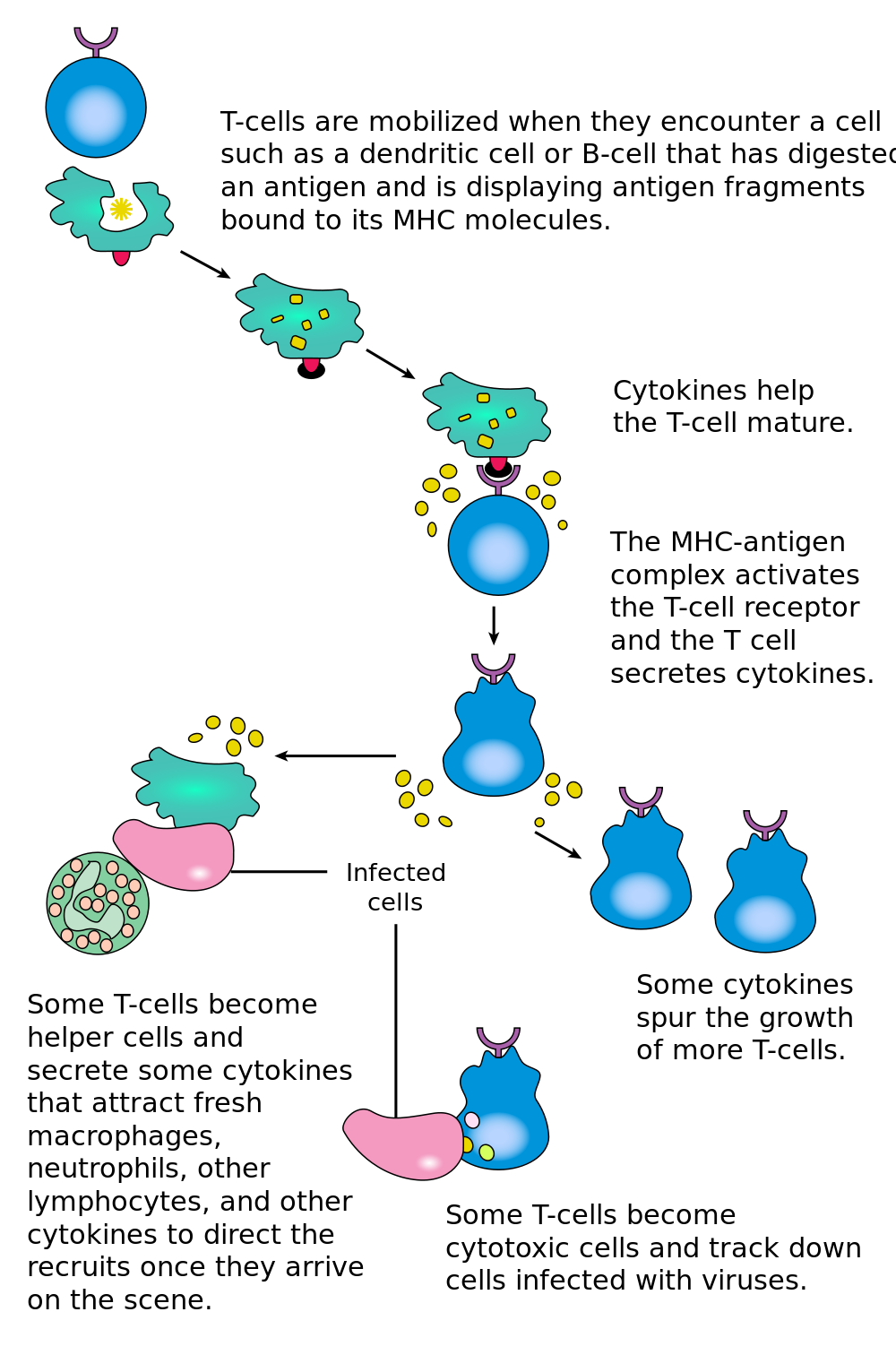
T cells must be activated to become either killer T cells or helper T cells. This requires presentation of a foreign antigen by antigen-presenting cells, as shown in Figure 17.5.2. Antigen-presenting cells may be dendritic cells, macrophages, or B cells. Activation occurs when T cells are presented with a foreign antigen coupled with an MHC self antigen. Helper T cells are more easily activated than killer T cells. Activation of killer T cells is strongly regulated and may require additional stimulation from helper T cells.
Killer T Cells
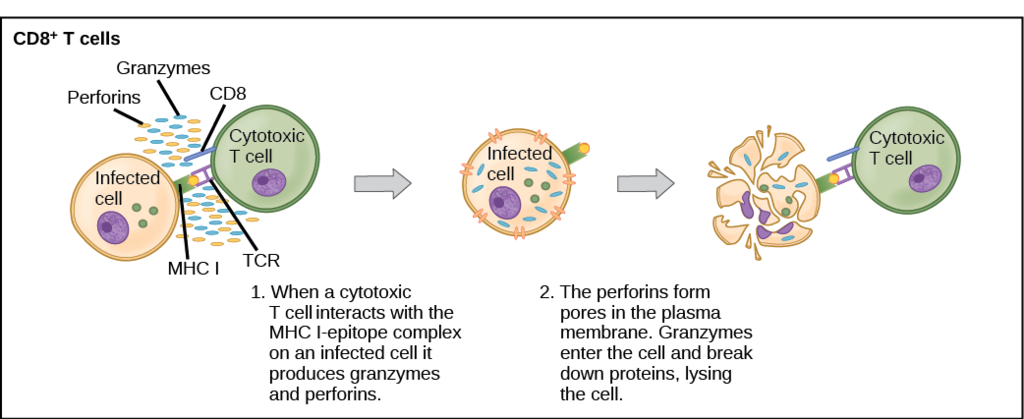
Activated killer T cells induce the death of cells that bear a specific non-self antigen because they are infected with pathogens or are cancerous. The antigen targets the cell for destruction by killer T cells, which travel through the bloodstream searching for target cells to kill. Killer T cells may use various mechanisms to kill target cells. One way is by releasing toxins in granules that enter and kill infected or cancerous cells (see Figure 17.5.3).
Helper T Cells
Activated helper T cells do not kill infected or cancerous cells. Instead, their role is to “manage” both innate and adaptive immune responses by directing other cells to perform these tasks. They control other cells by releasing cytokines, which are proteins that can influence the activity of many cell types, including killer T cells, B cells, and macrophages. Some cytokines released by helper T cells assist with the activation of killer T cells.
B Cells
B cells, or B lymphocytes, are the major cells involved in the creation of antibodies that circulate in blood plasma and lymph. Antibodies are large, Y-shaped proteins used by the immune system to identify and neutralize foreign invaders. Besides producing antibodies, B cells may also function as antigen-presenting cells, or secrete cytokines that help control other immune cells and responses.
B Cell Activation (or Antibody-Mediated Immunity)
Before B cells can actively function to defend the host, they must be activated. As shown in Figure 17.5.4, B cell activation begins when a B cell engulfs and digests an antigen. The antigen may be either free floating in the lymph, or it may be presented by an antigen-presenting cell, such as a dendritic cell or macrophage. In either case, the B cell then displays antigen fragments bound to its own MHC antigens. The MHC-antigen complex on the B cell attracts helper T cells. The helper T cells, in turn, secrete cytokines that help the B cell to multiply, and the daughter cells to mature into plasma cells.
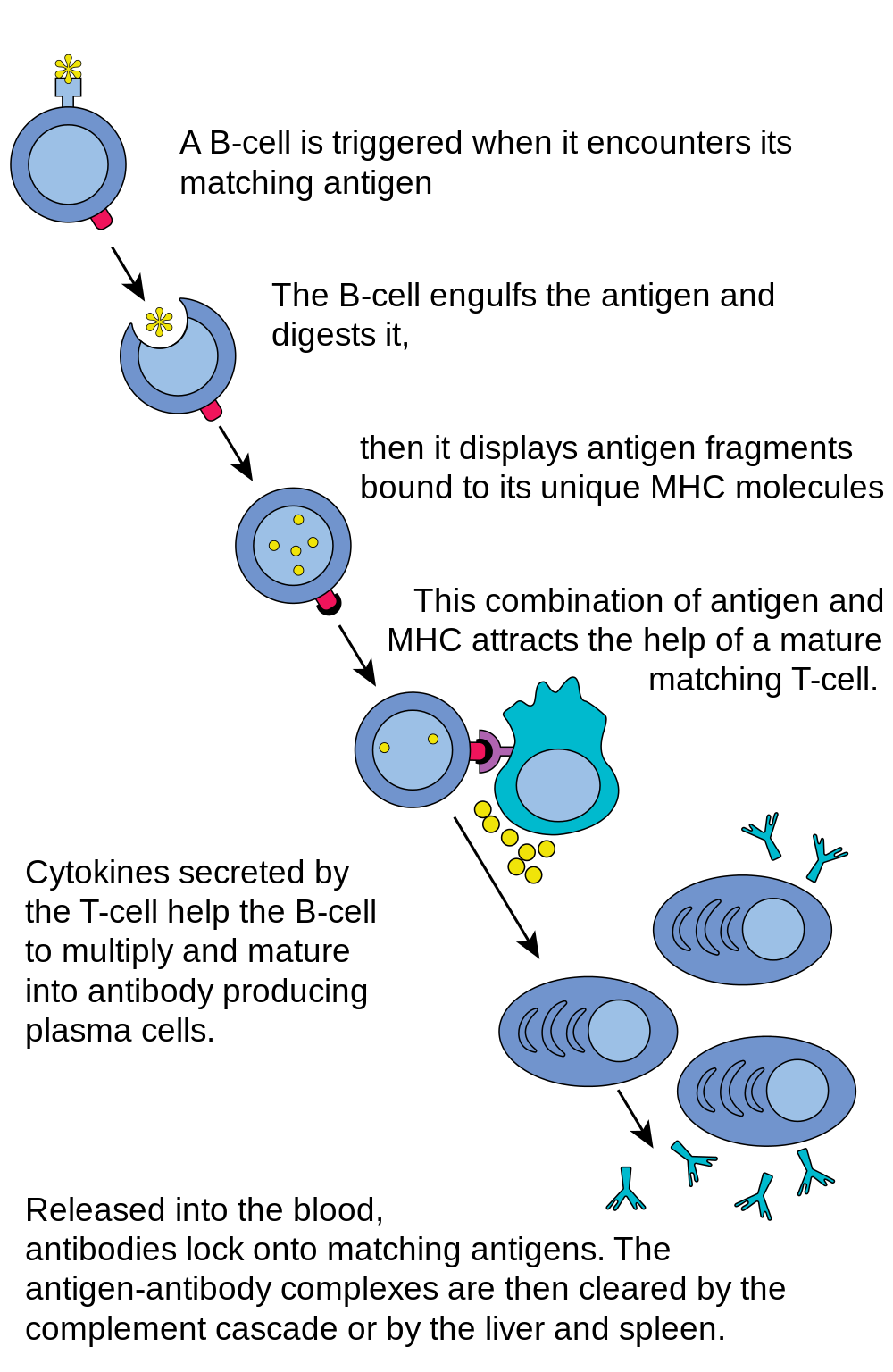
Plasma Cells
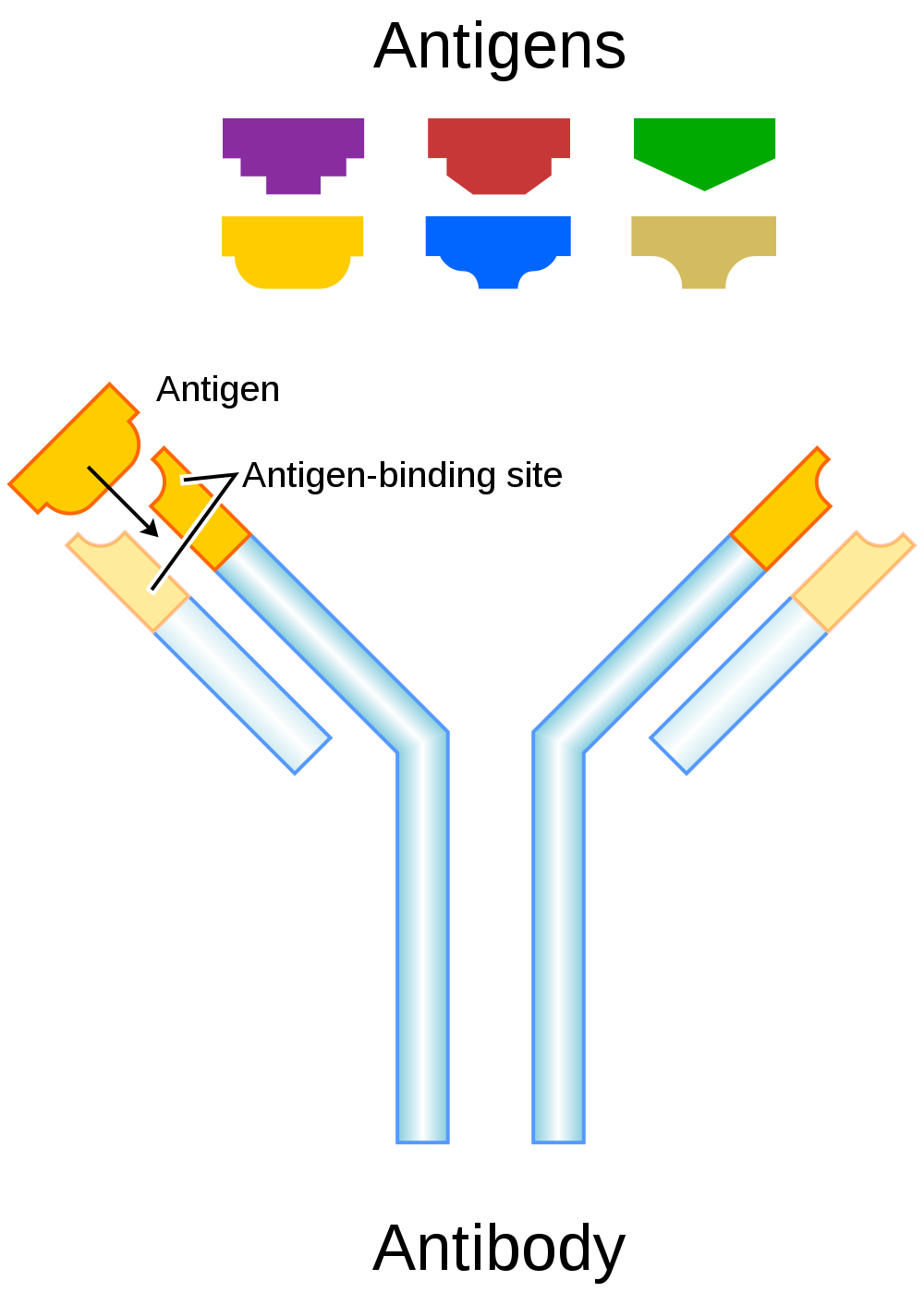
Plasma cells are antibody-secreting cells that form from activated B cells. Each plasma cell is like a tiny antibody factory. It may secrete millions of copies of an antibody, each of which can bind to the specific antigen that activated the original B cell. The specificity of an antibody to a specific antigen is illustrated in Figure 17.5.5. When antibodies bind with antigens, it makes the cells bearing them easier targets for phagocytes to find and destroy. Antibody-antigen complexes may also trigger the complement system of the innate immune system, which destroys the cells in a cascade of protein enzymes. In addition, the complexes are likely to clump together (agglutinate). If this occurs, they are filtered out of the blood in the spleen or liver.
Immunity
Once a pathogen has been cleared from the body, most activated T cells and B cells die within a few days. A few of the cells, however, survive and remain in the body as memory T cells or memory B cells. These memory cells are ready to activate an immediate response if they are exposed to the same antigen again in the future. This is the basis of immunity.
The earliest known reference to the concept of immunity relates to the bubonic plaque (see Figure 17.5.6). In 430 B.C., a Greek historian and general named Thucydides noted that people who had recovered from a previous bout of the plague could nurse people who were sick with the plague without contracting the illness a second time. We now know that this is true of many diseases, and that it occurs because of active immunity.

Active Immunity
Active immunity is the ability of the adaptive immune system to resist a specific pathogen because it has formed an immunological memory of the pathogen. Active immunity is adaptive, because it occurs during the lifetime of an individual as an adaptation to infection with a specific pathogen, and prepares the immune system for future challenges from that pathogen. Active immunity can come about naturally or artificially.
Naturally Acquired Active Immunity
Active immunity is acquired naturally when a pathogen invades the body and activates the adaptive immune system. When the initial infection is over, memory B cells and memory T cells remain, providing immunological memory of the pathogen. As long as the memory cells are alive, the immune system is ready to mount an immediate response if the same pathogen tries to infect the body again.
Artificially Acquired Active Immunity
Active immunity can also be acquired artificially through immunization. Immunization is the deliberate exposure of a person to a pathogen in order to provoke an adaptive immune response and the formation of memory cells specific to that pathogen. The pathogen is introduced in a vaccine — usually by injection, sometimes by nose or mouth (see Figure 17.5.7) — so immunization is also called vaccination.

Typically, only part of a pathogen, a weakened form of the pathogen, or a dead pathogen is used in a vaccine, which causes an adaptive immune response without making the immunized person sick. This is how you most likely became immune to diseases such as measles, mumps, and chicken pox. Immunizations may last for a lifetime, or they may require periodic booster shots to maintain immunity. While immunization generally has long-lasting effects, it usually takes several weeks to develop full immunity.
Immunization is the most effective method ever discovered of preventing infectious diseases. As many as 3 million deaths are prevented each year because of vaccinations. Widespread immunity from vaccinations is largely responsible for the worldwide eradication of smallpox, and the near elimination of several other infectious diseases from many populations, including polio and measles. Immunization is so successful because it exploits the natural specificity and inducibility of the adaptive immune system.
Passive Immunity
Passive immunity results when pathogen-specific antibodies or activated T cells are transferred to a person who has never been exposed to the pathogen. Passive immunity provides immediate protection from a pathogen, but the adaptive immune system does not develop immunological memory to protect the host from the same pathogen in the future. Unlike active immunity, passive immunity lasts only as long as the transferred antibodies or T cells survive in the blood — usually between a few days and a few months. However, like active immunity, passive immunity can be acquired both naturally and artificially.
Naturally Acquired Passive Immunity
Passive immunity is acquired naturally by a fetus through its mother’s blood. Antibodies are transported from mother to fetus across the placenta, so babies have high levels of antibodies at birth. Their antibodies have the same range of antigen specificities as their mother’s. Passive immunity may also be acquired by an infant through the mother’s breast milk. This gives young infants protection from common pathogens in their environment while their own immune system matures.
Artificially Acquired Passive Immunity
Older children and adults can acquire passive immunity artificially through the injection of antibodies or activated T cells, which may be done when there is a high risk of infection and insufficient time for the body to develop active immunity through vaccination. It may also be done to reduce symptoms of ongoing disease, or to compensate for immunodeficiency diseases.
Adaptive Immune Evasion
Many pathogens have been around for a long time, living with human populations for generations. To persist, some have evolved mechanisms to evade the adaptive immune system of human hosts. One way they have done this is by rapidly changing their non-essential antigens. This is called antigenic variation. An example of a pathogen that takes this approach is human immunodeficiency virus (HIV). It mutates rapidly so the proteins on its viral envelope are constantly changing. By the time the adaptive immune system responds, the virus’s antigens have changed. Antigenic variation is the main reason that efforts to develop a vaccine against HIV have not yet been successful.
Another evasion approach that some pathogens may take is to mask pathogen antigens with host molecules so the host’s immune system cannot detect the antigens. HIV takes this approach, as well. The envelope that covers the virus is formed from the outermost membrane of the host cell.
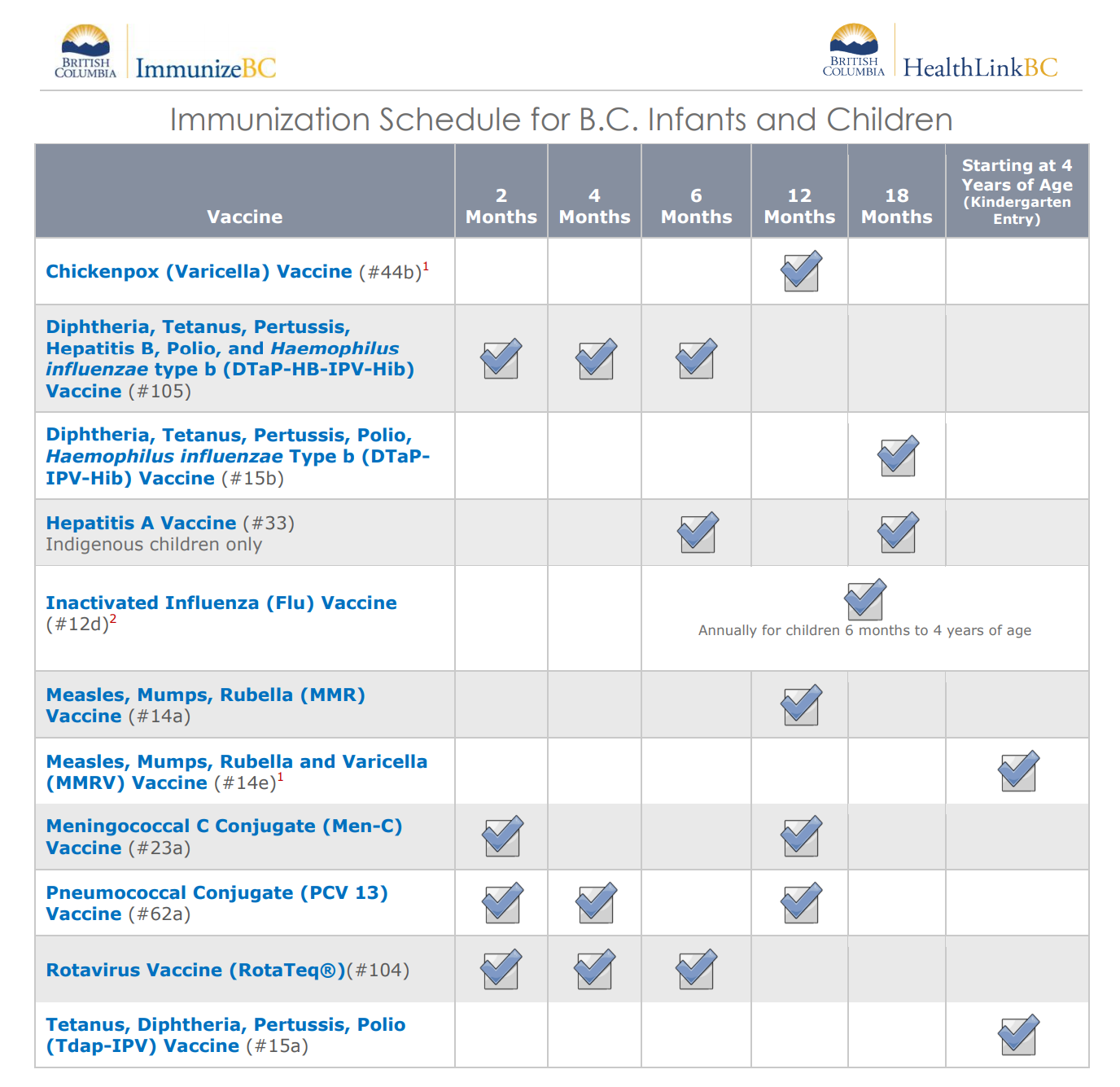
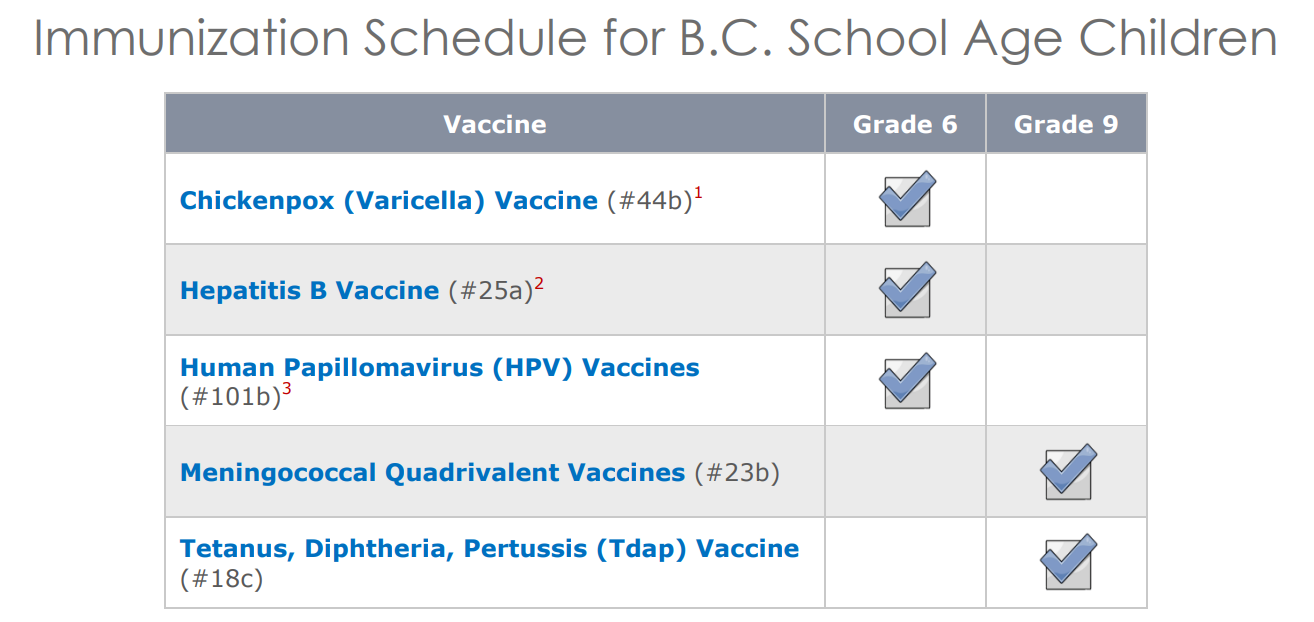
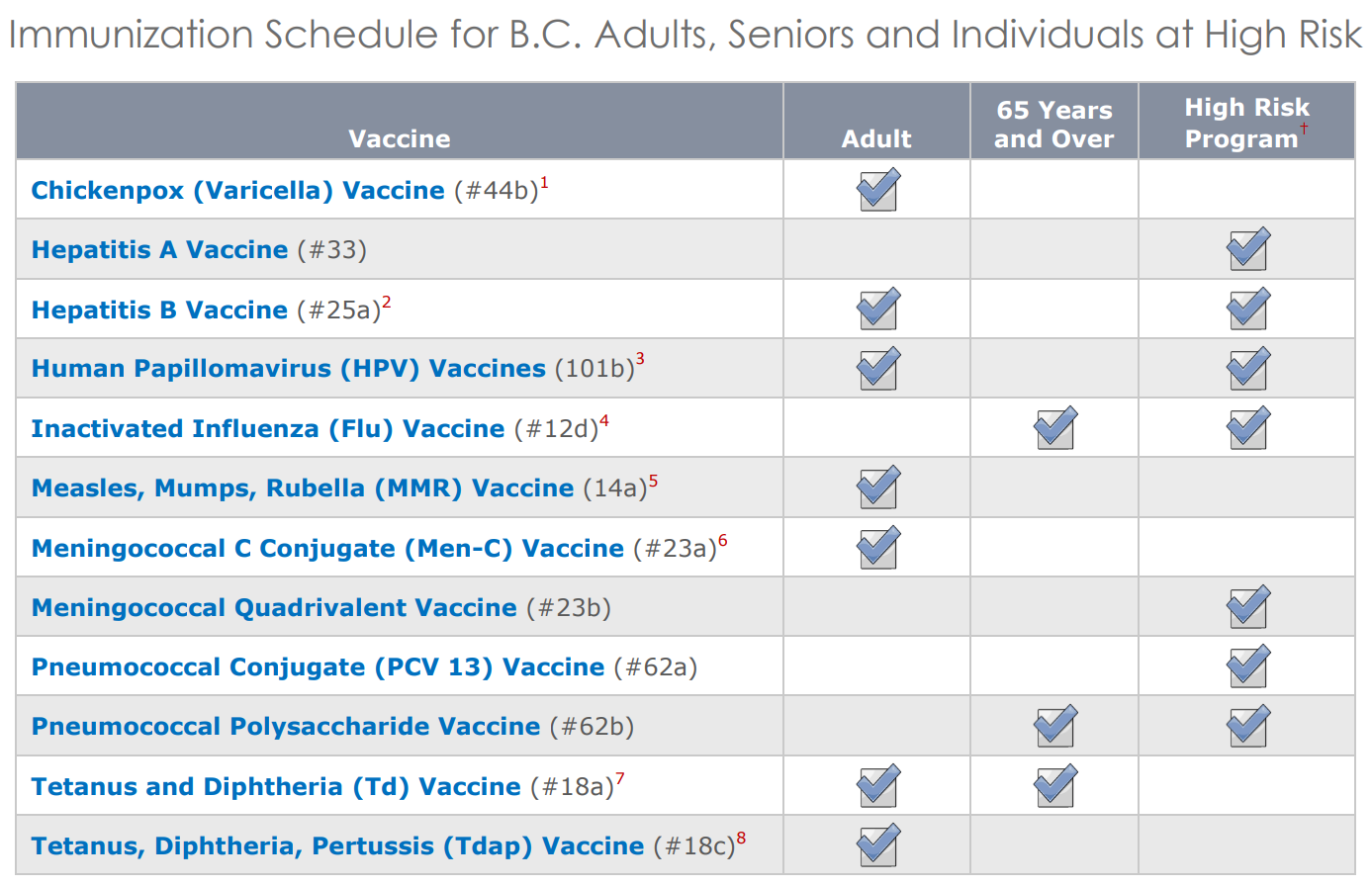
Feature: My Human Body
If you think that immunizations are just for kids, think again. There are several vaccines recommended by HealthLinkBC for people over the age of 18. The tables below from HealthLinkBC show the vaccine schedules recommended for infants and children, school-aged children, and adults and senior. Additional vaccines may be recommended for certain adults based on specific travel plans, medical conditions or other indications. Are you up to date with your vaccines? You can check with your doctor to be sure.
17.5 Summary
- The adaptive immune system is a subsystem of the overall immune system that recognizes and makes a tailored attack against specific pathogens or tumor cells. It is a slower, but more effective response than the innate immune response, and also leads to immunity to particular pathogens.
- Lymphocytes produced by the lymphatic system are the main cells of the adaptive immune system. There are two major types of lymphocytes: T cells and B cells. Both types must be activated by foreign antigens to become functioning immune cells.
- Most activated T cells become either killer T cells or helper T cells. Killer T cells destroy cells that are infected with pathogens or are cancerous. Helper T cells manage immune responses by releasing cytokines that control other types of leukocytes.
- Activated B cells form plasma cells that secrete antibodies, which bind to specific antigens on pathogens or infected cells. The antibody-antigen complexes generally lead to the destruction of the cells, for example, by attracting phagocytes or triggering the complement system.
- After an adaptive immune response occurs, long-lasting memory B cells and memory T cells may remain to confer immunity to the specific pathogen that caused the adaptive immune response. These memory cells are ready to activate an immediate response if they are exposed to the same antigen again in the future.
- Immunity may be active or passive. Active immunity occurs when the immune system has been presented with antigens that elicit an adaptive immune response. This may occur naturally as the result of an infection, or artificially as the result of immunization. Active immunity may last for years or even for life.
- Passive immunity occurs without an adaptive immune response by the transfer of antibodies or activated T cells. This may occur naturally between a mother and her fetus or her nursing infant, or it may occur artificially by injection. Passive immunity lasts only as long as the antibodies or activated T cells remain alive in the body, generally just weeks or months.
- Many pathogens have evolved mechanisms to evade the adaptive immune system. For example, human immunodeficiency virus (HIV) evades the adaptive immune system by frequently changing its antigens and by forming its outer envelope from the host’s cell membrane.
17.5 Review Questions
- What is the adaptive immune system?
- Define immunity.
-
- How are lymphocytes activated?
- Identify two common types of T cells and their functions.
- How do activated B cells help defend against pathogens?
- How does passive immunity differ from active immunity? How may passive immunity occur?
- What are two ways that active immunity may come about?
- What ways of evading the human adaptive immune system evolved in human immunodeficiency virus (HIV)?
- Why do vaccinations expose a person to a version of a pathogen?
17.5 Explore More
How do vaccines work? - Kelwalin Dhanasarnsombut, TED-Ed, 2015.
How we conquered the deadly smallpox virus - Simona Zompi, TED-Ed, 2013.
Why Do We Need A New Flu Shot Every Year? Seeker, 2015.
An HIV Vaccine: Mapping Uncharted Territory, NIAID, 2016.
Attributions
Figure 17.5.1
Killer_T_cells_surround_a_cancer_cell by Alex Ritter, Jennifer Lippincott Schwartz and Gillian Griffiths at the National Institutes of Health/ Visuals Online on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
Figure 17.5.2
T_cell_activation.svg by Rehua (derivative work) on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain). (Original image: T_cell_activation.png: from The Immune System - NIH Publication No. 03–5423)
Figure 17.5.3
Cytotoxic T Cell function by CNX OpenStax on Wikimedia Commons is used under a CC BY 4.0 (https://creativecommons.org/licenses/by/4.0) license.
Figure 17.5.4
B_cell_activation.svg by Fred the Oyster on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain). (Original from The Immune System - NIH Publication No. 03–5423)
Figure 17.5.5
Antibody.svg by Fvasconcellos on Wikimedia Commons is in the public domain (https://en.wikipedia.org/wiki/Public_domain). (Original black and white image from the National Human Genome Research Institute's Talking Genetics Glossary)
Figure 17.5.7
immunizations by U.S. Air Force photo by Airman 1st Class Destinee Dougherty from Military Health System website, Health.mil, is in the public domain (https://en.wikipedia.org/wiki/Public_domain).
References
HealthLinkBC. (2018). B.C. immunization schedules. Gov.BC.CA. https://www.healthlinkbc.ca/tools-videos/bc-immunization-schedules
Mayo Clinic Staff. (n.d.). Measles [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/measles/symptoms-causes/syc-20374857
Mayo Clinic Staff. (n.d.). Mumps [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/mumps/symptoms-causes/syc-20375361
Mayo Clinic Staff. (n.d.). Polio [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/polio/symptoms-causes/syc-20376512
Mayo Clinic Staff. (n.d.). Smallpox [online article]. MayoClinic.org. https://www.mayoclinic.org/diseases-conditions/smallpox/symptoms-causes/syc-20353027
NIAID. (2016, August 11). An HIV vaccine: Mapping uncharted territory. YouTube. https://www.youtube.com/watch?v=X-rC78MKZvw&feature=youtu.be
OpenStax. (2016, March 23). Figure 4 Naïve CD4+ T cells engage MHC II molecules on antigen-presenting cells (APCs) and become activated. Clones of the activated helper T cell, in turn, activate B cells and CD8+ T cells, which become cytotoxic T cells. Cytotoxic T cells kill infected cells [digital image]. In OpenStax, Biology (Section 42.2). OpenStax CNX. https://cnx.org/contents/GFy_h8cu@10.53:etZobsU-@6/Adaptive-Immune-Response
Seeker. (2015, September 2). Why do we need a new flu shot every year? YouTube. https://www.youtube.com/watch?v=5THf6gTNqO8
TED-Ed. (2015, January 12). How do vaccines work? - Kelwalin Dhanasarnsombut. YouTube. https://www.youtube.com/watch?v=rb7TVW77ZCs&feature=youtu.be
TED-Ed. (2013, October 28). How we conquered the deadly smallpox virus - Simona Zompi. YouTube. https://www.youtube.com/watch?v=yqUFy-t4MlQ&feature=youtu.be
A group of diseases involving abnormal cell growth with the potential to invade or spread to other parts of the body.
A structure within a cell, consisting of lipid bilayer. Vesicles form naturally during the processes of secretion, uptake and transport of materials within the plasma membrane.
A subset of the immune system that makes tailored attacks against specific pathogens or tumor cells such as the production of antibodies that match specific antigens.
The body system in humans and other animals that protects the organism by distinguishing foreign tissue and neutralizing potentially pathogenic organisms or substances.
A microorganism which causes disease.
Molecules on the surface of cells or viruses that the immune system identifies as either self (produced by your own body) or non-self (not produced by your own body).
The state of being immune from or insusceptible to a particular disease or the like. the condition that permits either natural or acquired resistance to disease. the ability of a cell to react immunologically in the presence of an antigen.
A type of leukocyte produced by the lymphatic system that is a key cell in the adaptive immune response to a specific pathogen or tumor cell.
a colorless cell that circulates in the blood and body fluids and is involved in counteracting foreign substances and disease; a white (blood) cell. There are several types, all amoeboid cells with a nucleus, including lymphocytes, granulocytes, monocytes, and macrophages.
A soft connective tissue in spongy bone that produces blood cells.
An organ of the lymphatic system where lymphocytes called T cells mature.
An organ of the lymphatic system where lymphocytes called T cells mature.
A secondary organ of the lymphatic system where blood and lymph are filtered.
One of many small structures located along lymphatic vessels where pathogens are filtered from lymph and destroyed by lymphocytes.
An antibody, also known as an immunoglobulin, is a large, Y-shaped protein produced mainly by plasma cells that is used by the immune system to neutralize pathogens such as pathogenic bacteria and viruses.
A type of lymphocyte that kills infected or cancerous cells (killer T cell) or helps regulate the immune response (helper T cell).
A T lymphocyte (a type of white blood cell), also known as a cytoxic T cell) that kills cancer cells, cells that are infected (particularly with viruses), or cells that are damaged in other ways.
A type of immune cell that stimulates killer T cells, macrophages, and B cells to make immune responses. A helper T cell is a type of white blood cell and a type of lymphocyte.
A type of immune cell that enables a T lymphocyte (T cell) to recognize an antigen and mount an immune response against the antigen. Antigen-presenting cells (APCs) include macrophages, dendritic cells, and B lymphocytes (B cells).
A special type of immune cell that is found in tissues, such as the skin, and boosts immune responses by showing antigens on its surface to other cells of the immune system. A dendritic cell is a type of phagocyte and a type of antigen-presenting cell (APC).
A large phagocytic cell found in stationary form in the tissues or as a mobile white blood cell, especially at sites of infection.
A type of white blood cell and, specifically, a type of lymphocyte.
Many B cells mature into what are called plasma cells that produce antibodies (proteins) necessary to fight off infections while other B cells mature into memory B cells.
Foreign proteins on the surface of a cell that triggers an immune response.
A subset of the immune system that makes generic attacks such as inflammation against invading pathogens.
A chemical released by injured, infected, or immune cells that triggers inflammation or other immune responses.
A straw-yellow fluid part of blood that contains many dissolved substances and blood cells.
A fluid that leaks out of capillaries into spaces between cells and circulates in the vessels of the lymphatic system.
A fully differentiated B cell that produces a single type of antibody.
A lymphocyte (B or T cell) that retains a “memory” of a specific pathogen after an infection is over and thus provides immunity to the pathogen.
The ability to resist a specific pathogen that results when an adaptive immune response to the pathogen produces memory lymphocytes for that pathogen.
The deliberate exposure of a person to a pathogen in order to provoke an immune response and the formation of memory cells specific to that pathogen.
Short-term immunity to a particular pathogen that results when antibodies or activated T cells are transferred to a person who has never been exposed to the pathogen.
A body system consisting of a network of tissues and organs that help rid the body of toxins, waste and other unwanted materials. The primary function of the lymphatic system is to transport lymph, a fluid containing infection-fighting white blood cells, throughout the body.
An innate immune response that consists of a cascade of proteins that complement the killing of pathogens by antibodies.
Either of two species of Lentivirus that infect humans. Over time, they cause acquired immunodeficiency syndrome, a condition in which progressive failure of the immune system allows life-threatening opportunistic infections and cancers to thrive.

