18.3 Structures of the Male Reproductive System
Created by CK-12 Foundation/Adapted by Christine Miller

Rocky Mountain Oysters
First, they are peeled and pounded flat. Then, they are coated in flour, seasoned with salt and pepper, and deep fried. What are they? They are often called Rocky Mountain oysters, but they don’t come from the sea. They may also be known as Montana tendergroin, cowboy caviar, or swinging beef — all names that hint at their origins. Here’s another hint: they are harvested only from male animals, such as bulls or sheep. What are they? In a word: testes.
Testes and Scrotum
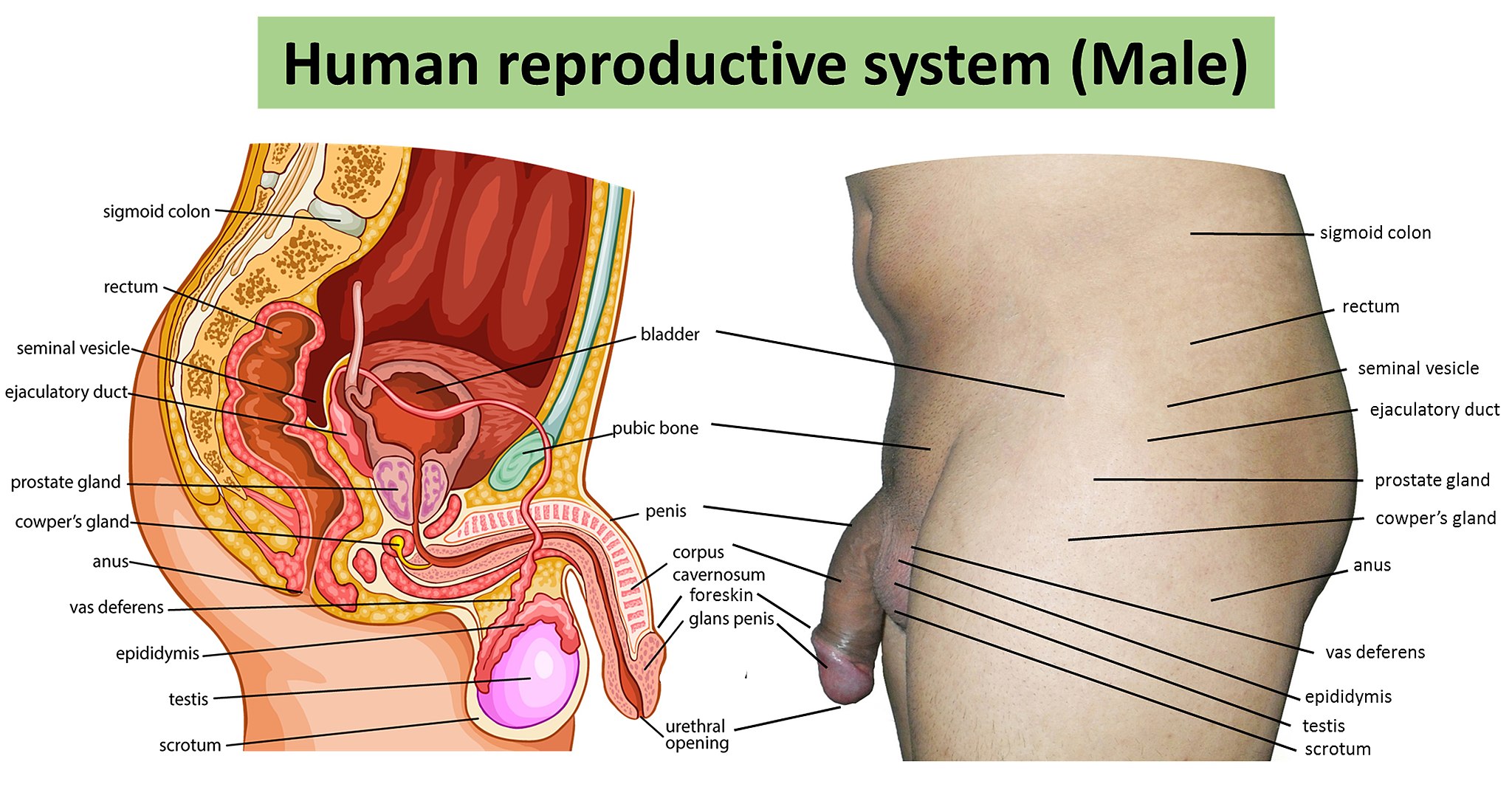
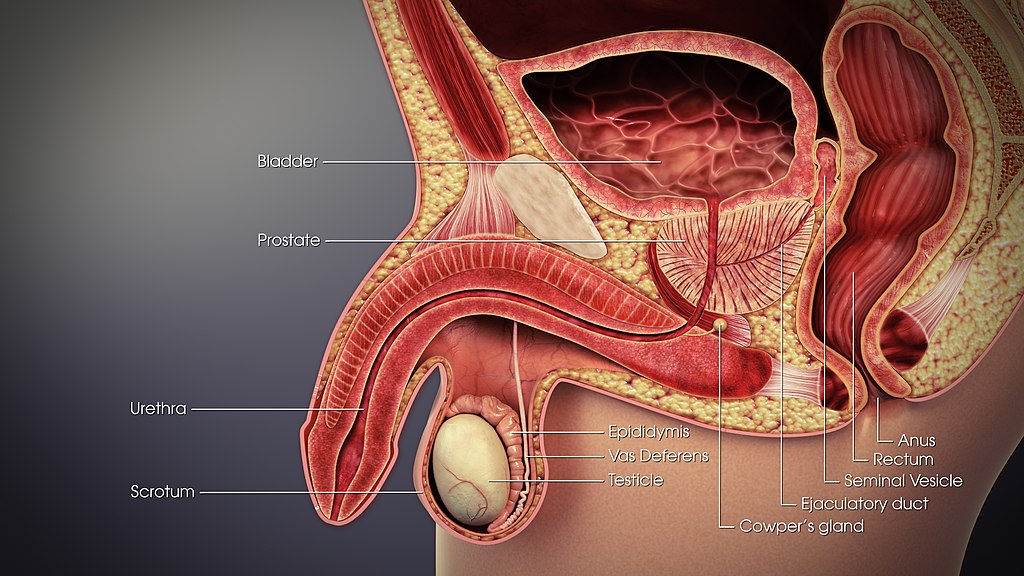
The two testes (singular, testis) are sperm– and testosterone-producing gonads in male mammals, including male humans. These and other organs of the human male reproductive system are shown in Figure 18.3.2. The testes are contained within the scrotum, a pouch made of skin and smooth muscle that hangs down behind the penis.
Testes Structure
The testes are filled with hundreds of tiny tubes, called seminiferous tubules, which are the functional units of the testes. As shown in the longitudinal-section drawing of a testis in Figure 18.3.3, the seminiferous tubules are coiled and tightly packed within divisions of the testis called lobules. Lobules are separated from one another by internal walls (or septa).
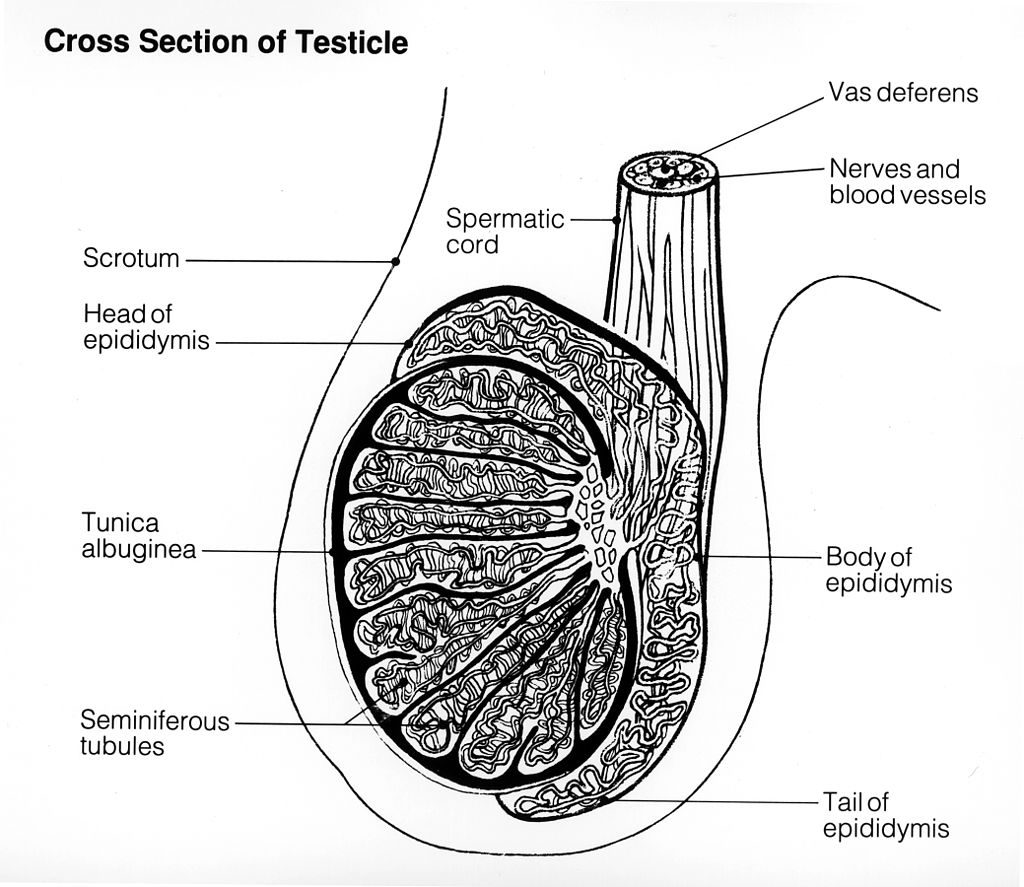
Tunica
The multi-layered covering of each testis, called the tunica, protects the organ, ensures its blood supply, and separates the testis into lobules. There are three layers of the tunica: the tunica vasculosa, tunica albuginea, and tunica vaginalis. The latter two layers are labeled in the drawing above (Figure 18.3.3).
- The tunica vasculosa is the innermost layer of the tunica. It consists of connective tissue and contains arteries and veins that carry blood to and from the testis.
- The tunica albuginea is the middle layer of the tunica. It is a dense layer of fibrous tissue that encases the testis. It also extends into the testis, creating the septa between lobules.
- The tunica vaginalis is the outmost layer of the tunica. It actually consists of two layers of tissue separated by a thin fluid layer. The fluid reduces friction between the testes and the scrotum.
Seminiferous Tubules
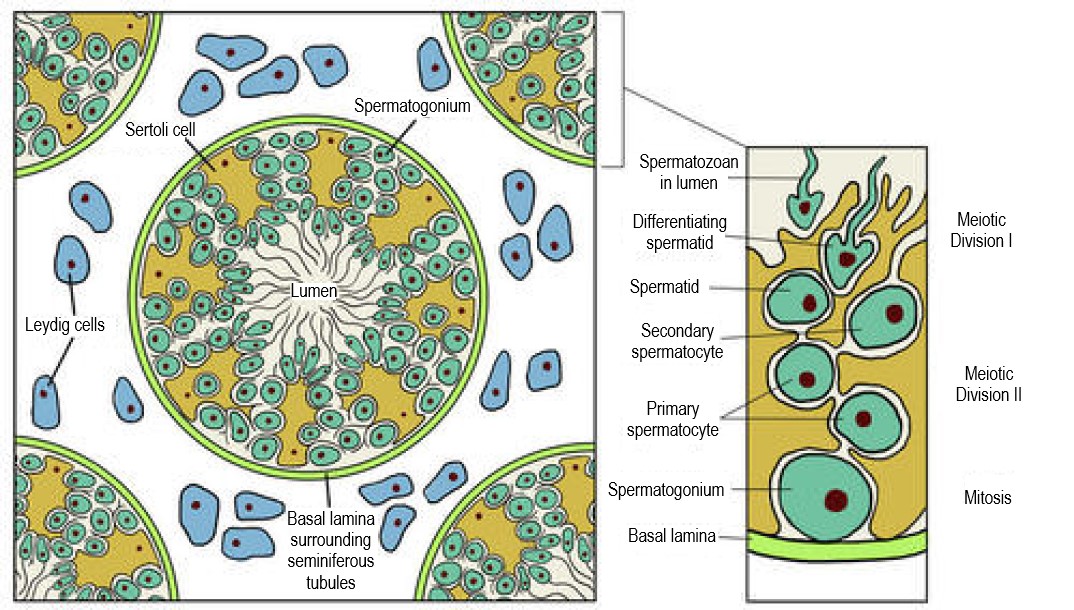
One or more seminiferous tubules are tightly coiled within each of the hundreds of lobules in the testis. A single testis normally contains a total of about 30 metres of these tightly packed tubules! As shown in the cross-sectional drawing of a seminiferous tubule in Figure 18.3.4, the tubule contains sperm in several different stages of development (spermatogonia, spermatocytes, spermatids, and spermatozoa). The seminiferous tubule is also lined with epithelial cells called Sertoli cells. These cells release a hormone (inhibin) that helps regulate sperm production. Adjacent Sertoli cells are closely spaced so large molecules cannot pass from the blood into the tubules. This prevents the male’s immune system from reacting against the developing sperm, which may be antigenically different from his own self tissues. Cells of another type, called Leydig cells, are found between the seminiferous tubules. Leydig cells produce and secrete testosterone.
Other Scrotal Structures
Besides the two testes, the scrotum also contains a pair of organs called epididymes (singular, epididymis) and part of each of the paired vas deferens (or ducti deferens). Both structures play important functions in the production or transport of sperm.
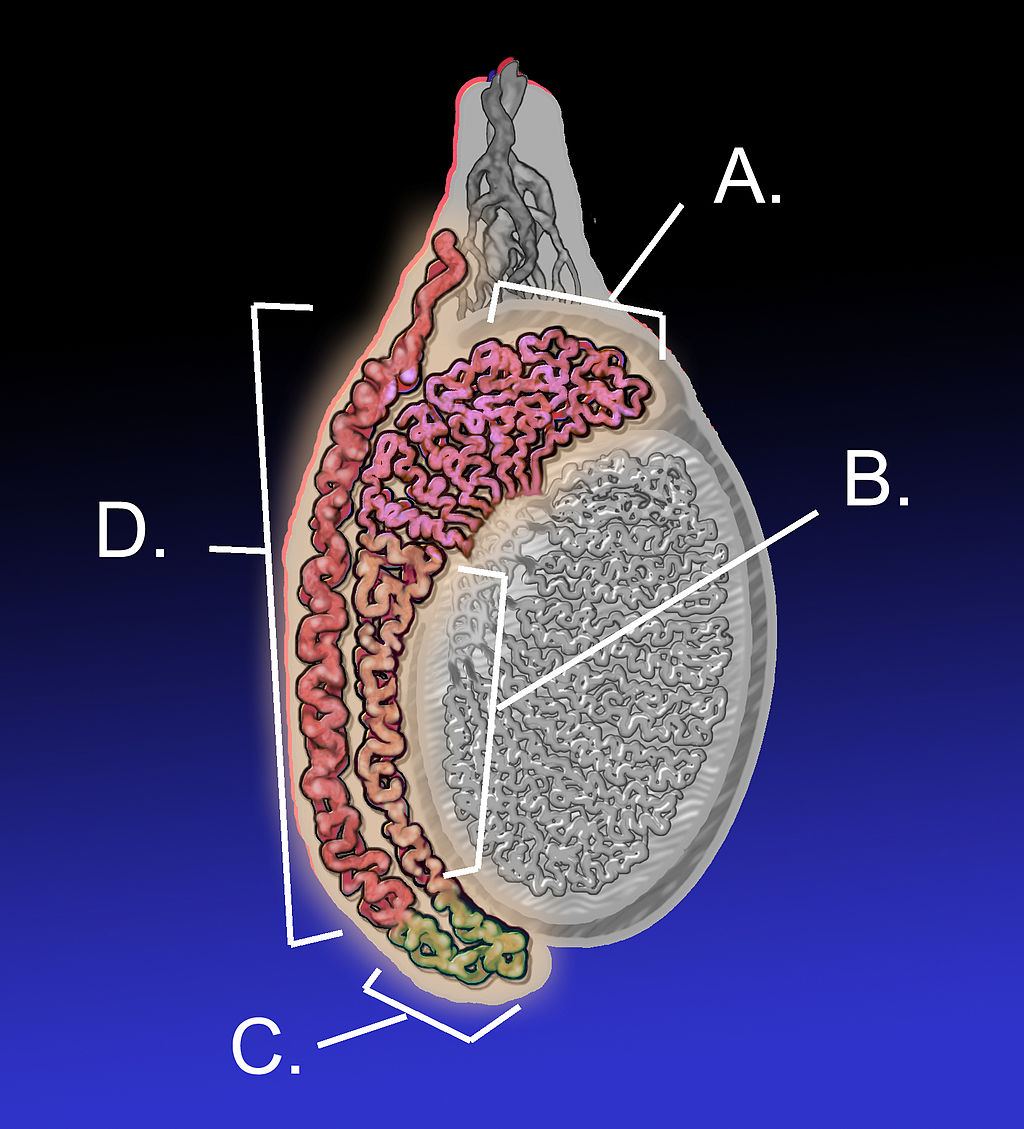
Epididymis
The seminiferous tubules within each testis join together to form ducts (called efferent ducts) that transport immature sperm to the epididymis associated with that testis. Each epididymis (plural, epididymes) consists of a tightly coiled tubule with a total length of about 6 metres. As shown in Figure 18.3.5, the epididymis is generally divided into three parts: the head (which rests on top of the testis), the body (which drapes down the side of the testis), and the tail (which joins with the vas deferens near the bottom of the testis). The functions of the two epididymes are to mature sperm, and then to store that mature sperm until they leave the body during an ejaculation, when they pass the sperm on to the vas deferens.
Vas Deferens
The vas deferens, also known as sperm ducts, are a pair of thin tubes, each about 30 cm (almost 12 in) long, which begin at the epididymes in the scrotum, and continue up into the pelvic cavity. They are composed of ciliated epithelium and smooth muscle. These structures help the vas deferens fulfill their function of transporting sperm from the epididymes to the ejaculatory ducts, which are accessory structures of the male reproductive system.
Accessory Structures
In addition to the structures within the scrotum, the male reproductive system includes several internal accessory structures that are shown in the detailed drawing in Figure 18.3.6. They include the ejaculatory ducts, seminal vesicles, and the prostate and bulbourethral (Cowper’s) glands.
Seminal Vesicles
The seminal vesicles are a pair of exocrine glands that each consist of a single tube, which is folded and coiled upon itself. Each vesicle is about 5 cm (almost 2 in) long and has an excretory duct that merges with the vas deferens to form one of the two ejaculatory ducts. Fluid secreted by the seminal vesicles into the ducts makes up about 70% of the total volume of semen, which is the sperm-containing fluid that leaves the penis during an ejaculation. The fluid from the seminal vesicles is alkaline, so it gives semen a basic pH that helps prolong the lifespan of sperm after it enters the acidic secretions inside the female vagina. Fluid from the seminal vesicles also contains proteins, fructose (a simple sugar), and other substances that help nourish sperm.
Ejaculatory Ducts
The ejaculatory ducts form where the vas deferens join with the ducts of the seminal vesicles in the prostate gland. They connect the vas deferens with the urethra. The ejaculatory ducts carry sperm from the vas deferens, as well as secretions from the seminal vesicles and prostate gland that together form semen. The substances secreted into semen by the glands as it passes through the ejaculatory ducts control its pH and provide nutrients to sperm, among other functions. The fluid itself provides sperm with a medium in which to “swim.”
Prostate Gland
The prostate gland is located just below the seminal vesicles. It is a walnut-sized organ that surrounds the urethra and its junction with the two ejaculatory ducts. The function of the prostate gland is to secrete a slightly alkaline fluid that constitutes close to 30% of the total volume of semen. Prostate fluid contains small quantities of proteins, such as enzymes. In addition, it has a very high concentration of zinc, which is an important nutrient for maintaining sperm quality and motility.
Bulbourethral Glands
Also called Cowper’s glands, the two bulbourethral glands are each about the size of a pea and located just below the prostate gland. The bulbourethral glands secrete a clear, alkaline fluid that is rich in proteins. Each of the glands has a short duct that carries the secretions into the urethra, where they make up a tiny percentage of the total volume of semen. The function of the bulbourethral secretions is to help lubricate the urethra and neutralize any urine (which is acidic) that may remain in the urethra.
Figure 18.3.7 Male reproductive system.
Penis
The penis is the external male organ that has the reproductive function of delivering sperm to the female reproductive tract. This function is called intromission. The penis also serves as the organ that excretes urine.
Structure of the Penis
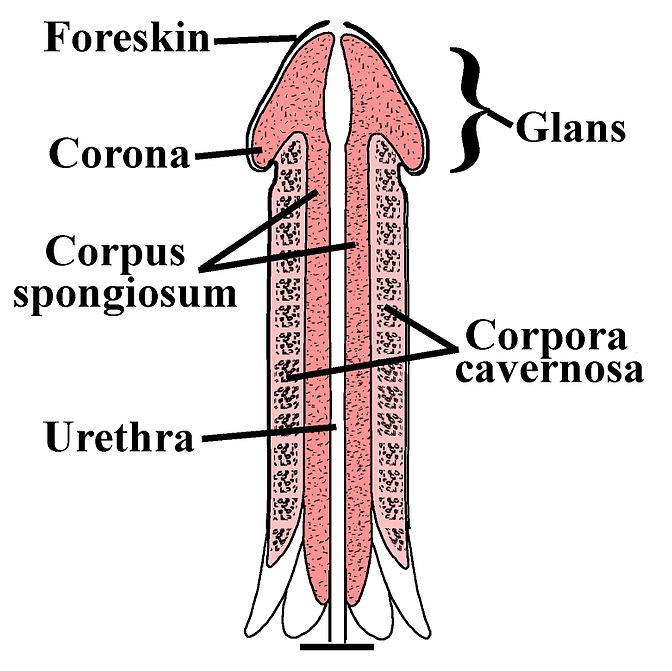
The structure of the penis and its location relative to other reproductive organs are shown in Figure 18.3.8. The part of the penis that is located inside the body and out of sight is called the root of the penis. The shaft of the penis is the part of the penis that is outside the body. The enlarged, bulbous end of the shaft is called the glans penis.
Urethra
The urethra passes through the penis to carry urine from the bladder — or semen from the ejaculatory ducts — through the penis and out of the body. After leaving the urinary bladder, the urethra passes through the prostate gland, where the urethra is joined by the ejaculatory ducts. From there, the urethra passes through the penis to its external opening at the tip of the glans penis. Called the external urethral orifice, this opening provides a way for urine or semen to leave the body.
Tissues of the Penis
The penis is covered with skin (epithelium) that is unattached and free to move over the body of the penis. In an uncircumcised male, the glans penis is also mainly covered by epithelium, which (in this location) is called the foreskin, and below which is a layer of mucous membrane. The foreskin is attached to the penis at an area on the underside of the penis called the frenulum.
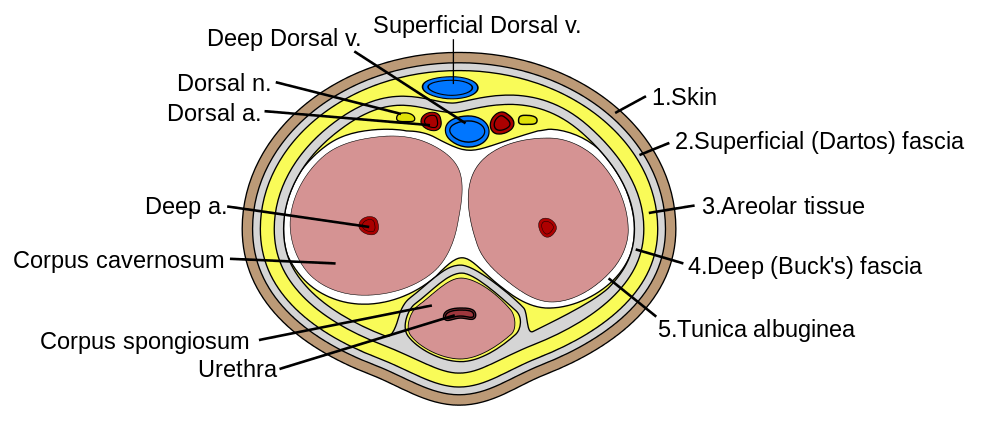
As shown in the Figure 18.3.9, the interior of the penis consists of three columns of spongy tissue that can fill with blood and swell in size, allowing the penis to become erect. This spongy tissue is called corpus cavernosum (plural, corpora cavernosa). Two columns of this tissue run side by side along the top of the shaft, and one column runs along the bottom of the shaft. The urethra runs through this bottom column of spongy tissue, which is sometimes called corpus spongiosum. The glans penis also consists mostly of spongy erectile tissue. Veins and arteries run along the top of the penis, allowing blood circulation through the spongy tissues.
Feature: Human Biology in the News
Lung, heart, kidney, and other organ transplants have become relatively commonplace, so when they occur, they are unlikely to make the news. However, when the nation’s first penis transplant took place, it was considered very newsworthy.
In 2016, Massachusetts General Hospital in Boston announced that a team of its surgeons had performed the first penis transplant in the United States. The patient who received the donated penis was a 64-year-old cancer patient. During the 15-hour procedure, the intricate network of nerves and blood vessels of the donor penis were connected with those of the penis recipient. The surgery went well, but doctors reported it would be a few weeks until they would know if normal urination would be possible, and even longer before they would know if sexual functioning would be possible. At the time that news of the surgery was reported in the media, the patient had not shown any signs of rejecting the donated organ. Within 6 months, the patient was able to urinate properly and was beginning to regain sexual function. The surgeons also reported they were hopeful that such transplants would become relatively common, and that patient populations would expand to include wounded warriors and transgender males seeking to transition.
The 2016 Massachusetts operation was not the first penis transplant ever undertaken. The world’s first successful penis transplant was actually performed in 2014 in Cape Town, South Africa. A young man who had lost his penis from complications of a botched circumcision at age 18 was given a donor penis three years later. That surgery lasted nine hours and was highly successful. The young man made a full recovery and regained both urinary and sexual functions in the transplanted organ.
In 2005, a man in China also received a donated penis in a technically successful operation. However, the patient asked doctors to reverse the procedure just two weeks later, because of psychological problems associated with the transplanted organ for both himself and his wife.
18.3 Summary
- The two testes are sperm– and testosterone-producing male gonads. They are contained within the scrotum, a pouch that hangs down behind the penis. The testes are filled with hundreds of tiny, tightly coiled seminiferous tubules, where sperm are produced. The tubules contain sperm in different stages of development and also Sertoli cells, which secrete substances needed for sperm production. Between the tubules are Leydig cells, which secrete testosterone.
- Also contained within the scrotum are the two epididymes. Each epididymis is a tightly coiled tubule where sperm mature and are stored until they leave the body during an ejaculation.
- The two vas deferens are long, thin tubes that run from the scrotum up into the pelvic cavity. During ejaculation, each vas deferens carries sperm from one of the two epididymes to one of the pair of ejaculatory ducts.
- The two seminal vesicles are glands within the pelvis that secrete fluid through ducts into the junction of each vas deferens and ejaculatory duct. This alkaline fluid makes up about 70% of semen, the sperm-containing fluid that leaves the penis during ejaculation. Semen contains alkaline substances and nutrients that sperm need to survive and “swim” in the female reproductive tract.
- The paired ejaculatory ducts form where the vas deferens joins with the ducts of the seminal vesicles in the prostate gland. They connect the vas deferens with the urethra. The ejaculatory ducts carry sperm from the vas deferens, as well as secretions from the seminal vesicles and prostate gland that together form semen.
- The prostate gland is located just below the seminal vesicles, and it surrounds the urethra and its junction with the ejaculatory ducts. The prostate secretes an alkaline fluid that makes close to 30% of semen. Prostate fluid contains a high concentration of zinc, which sperm need to be healthy and motile.
- The paired bulbourethral glands are located just below the prostate gland. They secrete a tiny amount of fluid into semen. The secretions help lubricate the urethra and neutralize any acidic urine it may contain.
- The penis is the external male organ that has the reproductive function of intromission, which is delivering sperm to the female reproductive tract. The penis also serves as the organ that excretes urine. The urethra passes through the penis and carries urine or semen out of the body. Internally, the penis consists largely of columns of spongy tissue that can fill with blood and make the penis stiff and erect. This is necessary for sexual intercourse so intromission can occur.
18.3 Review Questions
-
-
- Describe the structure of a testis.
- Which parts of the male reproductive system are connected by the ejaculatory ducts? What fluids enter and leave the ejaculatory ducts?
- A vasectomy is a form of birth control for men that is performed by surgically cutting or blocking the vas deferens so that sperm cannot be ejaculated out of the body. Do you think men who have a vasectomy emit semen when they ejaculate? Why or why not?
-
18.3 Explore More
Human Physiology – Functional Anatomy of the Male Reproductive System (Updated), Janux, 2015.
The Science of ‘Morning Wood’, AsapSCIENCE, 2012.
I Had One Of The World’s First Penis Transplants – Thomas Manning | This Morning, 2016.
Attributions
Figure 18.3.1
Lamb_fries by Paul Lowry on Wikimedia Commons is used under a CC BY 2.0 (https://creativecommons.org/licenses/by/2.0) license.
Figure 18.3.2
Human_reproductive_system_(Male) by Baresh25 on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 18.3.3
Testicle by Unknown Illustrator from National Cancer Institute, of the National Institutes of Health, Visuals Online, ID 1769 is in the public domain (https://en.wikipedia.org/wiki/en:public_domain).
Figure 18.3.4
Testis-cross-section by Laura Guerin from CK-12 Foundation is used under a
CC BY-NC 3.0 (https://creativecommons.org/licenses/by-nc/3.0/) license.
Figure 18.3.5
Epididymis-KDS by KDS444 on Wikimedia Commons is used under a CC BY-SA 3.0 (https://creativecommons.org/licenses/by-sa/3.0) license.
Figure 18.3.6
3D_Medical_Animation_Vas_Deferens by https://www.scientificanimations.com/wiki-images (image 26 of 191) on Wikimedia Commons is used under a CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0) license.
Figure 18.3.7
Male anatomy blank [adapted] by Tsaitgaist on Wikimedia Commons is used and adapted by Christine Miller under a CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0/) license. (Original: Male anatomy.png)
Figure 18.3.8
Penile-Clitoral_Structure by Esseh on Wikimedia Commons is used under a CC BY-SA 3.0 (http://creativecommons.org/licenses/by-sa/3.0/) license.
Figure 18.3.9
Penis_cross_section.svg by Mcstrother on Wikimedia Commons is used under a CC BY 3.0 (https://creativecommons.org/licenses/by/3.0) license.
References
AsapSCIENCE, (2012, November 14). The science of ‘morning wood’. YouTube. https://www.youtube.com/watch?v=D1et5NgT6bQ&feature=youtu.be
Associated Press. (2016, May 17). Man receives new penis in 15-hour operation, the first transplant of its kind in U.S. history [online article]. Canada.com. http://www.canada.com/health/receives+penis+hour+operation+first+transplant+kind+history/11922832/story.html
Brainard, J/ CK-12 Foundation. (2012). Figure 3 Cross section of a testis and seminiferous tubules [digital image]. In CK-12 Biology (Section 25.1) [online Flexbook]. CK12.org. https://www.ck12.org/book/ck-12-biology/section/25.1/
Gallagher, J. (2015, March 13). South Africans perform first ‘successful’ penis transplant (online article). BBC News. https://www.bbc.com/news/health-31876219
Grady, D. (2016, May 16). Cancer survivor receives first penis transplant in the United States [online article]. New York Times. https://www.nytimes.com/2016/05/17/health/thomas-manning-first-penis-transplant-in-us.html
Janux. (2015, August 16). Human physiology – Functional anatomy of the male reproductive system (Updated). YouTube. https://www.youtube.com/watch?v=k60M1h-DKVY&feature=youtu.be
This Morning. (2016, June 15). I had one of the world’s first penis transplants – Thomas Manning | This Morning. YouTube. https://www.youtube.com/watch?v=Ot7CYjm9B7U&feature=youtu.be
Two male reproductive organs that produce sperm and secrete testosterone; male gonad.
The male reproductive cell.
The male sex hormone secreted mainly by the testes.
A pouch-like external structure of the male reproductive system, located behind the penis, that contains the testes, epididymes, and part of the vas deferens.
The male reproductive organ containing the urethra, through which semen and urine pass out of the body.
One of the many tiny tubes contained within the testes where sperm are produced.
The innermost layer of the tunica of the testes. It consists of connective tissue and contains arteries and veins that carry blood to and from the testis.
The middle layer of the tunica of the testes. It is a dense layer of fibrous tissue that encases the testis. It also extends into the testis, creating the septa between lobules.
The outmost layer of the tunica of the testes. It actually consists of two layers of tissue separated by a thin layer of serous fluid which reduces friction between the testes and the scrotum.
A type of cell that lines the seminiferous tubules in the testes and plays several roles in sperm production.
A gonadal hormone which inhibits the secretion of follicle-stimulating hormone, under consideration as a potential male contraceptive.
A type of cell found between seminiferous tubules in the testes that produces and secretes testosterone.
One of two male reproductive organs where sperm mature and are stored until they leave the body during ejaculation.
One of a pair of thin tubes that transports sperm from an epididymis to an ejaculatory duct during ejaculation; also called sperm duct.
A body cavity that is bounded by the bones of the pelvis. Its oblique roof is the pelvic inlet (the superior opening of the pelvis). Its lower boundary is the pelvic floor. The pelvic cavity primarily contains reproductive organs, the urinary bladder, the pelvic colon, and the rectum.
An involuntary, nonstriated muscle that is found in the walls of internal organs such as the stomach.
One of two tubes in the male reproductive system that joins the vas deferens with the urethra and carries semen during ejaculation.
One of a pair of glands of the male reproductive system that secretes fluid into semen.
Fluid containing sperm and glandular secretions, which nourishes sperm and carries them through the urethra and out of the body.
The process in males in which muscle contractions propel sperm from the epididymes and out through the urethra in semen.
A measure of the acidity or basicity of aqueous or other liquid solutions. The term translates the values of the concentration of the hydrogen ion in a scale ranging from 0 and 14. In pure water, which is neutral (neither acidic nor alkaline), the concentration of the hydrogen ion corresponds to a pH of 7. A solution with a pH less than 7 is considered acidic; a solution with a pH greater than 7 is considered basic, or alkaline.
The female reproductive organ that receives sperm during sexual intercourse and provides a passageway for a baby to leave the mother’s body during birth.
A gland in the male reproductive system that secretes fluid into semen and provides nourishing substances to sperm.
A tube-like organ of the urinary system that carries urine out of the body from the bladder and, in males, also carries semen out of the body.
One of a pair of glands in the male reproductive system that secretes a fluid to help lubricate the urethra and neutralize any urine it may contain before ejaculation occurs (also called Cowper’s gland).
The retractable roll of skin covering the end of the penis.
Epithelial tissue that lines inner body surfaces and body openings and produces mucus.
The location where the foreskin meets the underside of the penis. It looks like a small V just below the glans. Usually part of it remains after circumcision.
Either of two masses of erectile tissue forming the bulk of the penis and the clitoris.
A mass of erectile tissue alongside the corpora cavernosa of the penis and terminating in the glans.
The rounded head (or tip) of the penis.
A type of blood vessel that carries blood toward the heart from the lungs or body.
A type of blood vessel that carries blood away from the heart and toward the lungs or body.
One of a pair of organs that secrete sex hormones and produce gametes; testis in males and ovary in females.
A liquid waste product of the body that is formed by the kidneys and excreted by the other organs of the urinary system.
The physical activity of sex between two people.


